A sinister source of gastrointestinal bleeding treated by transhepatic splenic varix embolization in a paediatric patient: a case report
Introduction
Left-sided, or sinistral portal hypertension (SPH) is a rare but well-documented complication of pancreatic disease. Adult cases have been described in relation to pancreatic pathologies. The most common causes include chronic pancreatitis, pancreatic pseudocysts and pancreatic tumors. It has been described less commonly in relation to trauma, splenic vein injury post-liver transplant, gastric or renal pathologies and retroperitoneal tumors (1,2). Diagnostic features of SPH include splenomegaly, isolated gastric varices and the absence of liver pathology. Gastrointestinal bleeding (GIB) is a common feature.
Pancreatic disease usually leads to localized inflammation and in turn can result in thrombosis of the splenic vein. This leads to back pressure that is transmitted to the gastric and gastroepiploic veins through anastomoses and increases the pressure on the left side of the portal system. The increased blood flow to the vena cava via the stomach and the pressure in the gastric fundus results in isolated gastric varices. Blood moves to the portal vein via the gastric coronary veins and the portal vein enlarges causing SPH without liver injury (1,3).
Treatment avenues remain controversial. In the past splenectomy was offered to most patients, especially those with significant thrombocytopenia or symptomatic disease, and is curative. At present less-invasive procedures such as splenic artery embolization or placement of coils are preferred in clinically stable patients (1-7).
We present the following case in accordance with the CARE reporting checklist (available at https://dx.doi.org/10.21037/pm-21-30).
Case presentation
We present the case of a 15-year-old male with recurrent episodes of intermittent occult GIB associated with epigastric pain manifesting at 10 years of age. He was diagnosed with hereditary pancreatitis (one copy of the N29I mutation in PRSS1) at 2.5 years. His father and sister share the same mutation. The patient developed multiple episodes of acute pancreatitis resulting in a pancreatic pseudocyst and exocrine pancreas insufficiency diagnosed by 5 years of age. Fat soluble vitamins, pancreatic enzymes and a proton-pump inhibitor (PPI) have been prescribed for a decade.
His course was complicated by anemia requiring multiple blood transfusions and iron supplementation. He developed thrombocytopenia (100×109/L which slowly dropped to 83×109/L over 24 months) with no hematologic etiology.
Investigations over 24 months included negative stool cultures and 2 negative Meckel’s scans, 2 tagged red blood cell scans, multiple upper endoscopies and colonoscopies, a diagnostic laparoscopy, and a capsule endoscopy which did not identify varices, active bleeding or other abnormalities. Despite these findings, an obscure variceal bleed was suspected to be the source of intermittent hematochezia. Abdominal ultrasound (AUS) showed splenomegaly (15 cm) and normal liver anatomy. A 2-month trial of empiric nadolol was given to prevent episodes of bleeding which provided temporary benefit, however hematochezia recurred while he was on this therapy and it was discontinued.
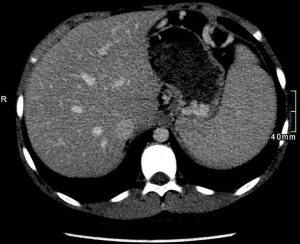
Contrast enhanced CT (Figure 1) showed hepatosplenomegaly, prominence of the short gastric veins near the splenic hilum and narrowing of the splenic vein without liver pathology.
A working diagnosis of SPH was made based on radiographic results, clinical manifestation and past medical history.
Push enteroscopy identified a small area of active bleeding in the distal ileum and 20 centimeters of bowel was resected by General Surgery, with the terminal ileum and ileocecal valve remaining intact. Histological assessment revealed the source of bleed was likely due to surgical manipulation and not a vascular malformation. A subsequent CT scan re-demonstrated splenomegaly and short gastric and mesenteric varices in keeping with the previous splenic vein occlusion. The splenic vein was patent and no thrombi were detected in other vessels. A heparin challenge was normal.
At the age of 12 years, and after 4 hospital admissions, Interventional Radiology (IR) performed a mesenteric angiogram for splenic artery embolization with micro-coil placement. There was evidence of short gastric and mesenteric varices. He was asymptomatic for 2 years following this intervention and remained on a PPI and iron supplements. Subsequent ultrasounds demonstrated resolution of the previously noted varices and splenic length decreased to 12–13 cm. Prior to this procedure the patient had long standing thrombocytopenia with a nadir of 83×109/L but since intervention it has remained stable at approximately 121×109/L.
At the age of 14-year-old the patient was admitted for GIB again requiring transfusion. Push enteroscopy did not identify a source of bleeding. Repeat abdominal CT showed gastric and mesenteric varices and splenomegaly with a short segment of splenic vein occlusion at the splenic hilum. Portal circulation was unobstructed. Transient elastography of the liver showed no signs of cirrhosis.
The suspected cause of GIB was a mesenteric or gastric varix that developed secondary to sinistral portal hypertension. The mechanism of pathology can be described by chronic parenchymal loss of the pancreatic body and tail causing narrowing of the main splenic vein. Splenomegaly caused backflow and engorged portal veins, predominantly in the gastro-omental and short gastric veins. There was absence of bowel pathology, a portosystemic shunt, liver disease or absence of systemic venous drainage obstruction that could be related to portal hypertension.
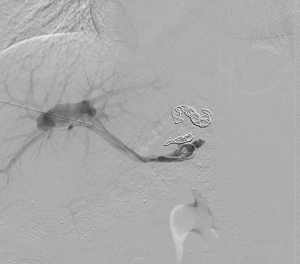
An interdisciplinary team meeting including IR, Surgery and GI was held to discuss this challenging case. Transhepatic splenic varix embolization was completed without complication (Figures 2,3). There was a plan to re-canalize the splenic vein thrombus, however spasm of the vessel occurred and the procedure was aborted. Unfortunately, portal venous pressure was not documented.

He was commenced on an indefinite course of empiric nadolol (30 mg once daily) as a prophylactic measure to prevent recurrent GIB. His condition has been stable since this intervention was initiated more than 24 months ago. Spleen size has remained stable at about 14 cm in length, platelet count remains 120×109/L and no further bleeding has occurred, presumably due to gastric and omental variceal blood flow that has been constricted with the use of nadolol.
Should hemorrhage recur, further management options include splenectomy for permanent cure of the varices versus reattempting to recanalizing the splenic vein.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s substitute decision maker for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
SPH is a rare though well-documented complication of pancreatic disease. A diagnosis of SPH can be made when there is radiological evidence of splenic vein occlusion after cirrhosis and extrahepatic portal vein occlusion have been ruled out. Diagnosing SPH is notoriously difficult and often requires an extensive work-up and involvement from a multi-disciplinary team (1-3).
To our knowledge, we present the first case report of SPH in a paediatric patient secondary to hereditary pancreatitis.
An extensive literature review described 3 cases of paediatric SPH associated with GIB, splenomegaly and gastric varices. Only one was associated with pancreatic pathology (8). In that scenario, a 9-year-old boy developed SPH, splenomegaly and gastric and duodenal varices 11 months after the removal of a pancreatoblastoma. He was treated with partial splenic arterial embolization with good response (8). The other 2 scenarios with normal pancreatic function are of a 10-year-old girl and an 8-year-old boy. The 10-year-old girl had a reactive lymph node compressing the splenic vein, causing splenomegaly, gastric varices and life-threatening hemorrhage. She underwent splenic artery embolization which resolved the bleeding episodes (1). The 8-year-old boy had developed recurrent upper GIB secondary to a splenic vein thrombus due to paroxysmal nocturnal hemoglobinuria (9). In both of these cases splenectomy was the eventual treatment choice which ended any further bleeding.
Interestingly, there is one historic case reported in 1971 about a family with hereditary pancreatitis. Though not explicitly diagnosed, the description of a 30-year-old man is reminiscent of SPH secondary to hereditary pancreatitis. He had a long-standing history of recurrent episodes of pancreatitis with calcification, recurrent GIB, thrombocytopenia, normal liver biopsy and gastric varices and multiple family members with recurrent epigastric pain and pancreatic insufficiency (10).
The management of variceal bleeding related to sinistral portal hypertension is primarily based on adult literature. There is no definitive consensus for the treatment of this disorder.
Splenectomy has been the long-standing definitive cure for bleeding caused by gastric varices related to SPH (1-9). This source of increased venous backpressure is removed and varices do not form. Recent studies recommend splenectomy when there is acute or uncontrollable gastrointestinal hemorrhage or intractable bleeding despite other interventions. This procedure infers a lifelong risk of infection by encapsulated organisms. Each patient must be fully immunized with the pneumococcal, meningococcal and Hemophilus influenza vaccines.
Splenic arterial embolization using coils is another treatment modality used to treat this disorder (1-9). It is often reserved for hemodynamically stable patients. This method is a minimally invasive procedure which occludes the main splenic artery and decreases splenic perfusion. Risks of this procedure include potential infarct of the stomach and pancreas due to shared blood supply and infection, often treated prophylactically with antibiotics.
Non-selective beta-blockers such as nadolol and propranolol are routinely used for prophylaxis for esophageal varices caused by portal hypertension. Currently there is no data that suggests that the use of a nadolol is protective against subsequent hemorrhage or splenectomy in patients with gastric varices or SPH. We decided to treat our patient empirically with nadolol in an attempt to avoid future splenectomy as we believed the pressure in the gastric varices would respond in a similar manner to esophageal varices. He has been symptom free for 10 months.
Overall, treatment for children and adults with variceal bleeding secondary to SPH is difficult to determine and should be individualized and discussed in interdisciplinary team meetings to optimize the outcome for the patient. Splenectomy may be useful in patients who are critically ill or who have prior thrombocytopenia (3), and splenic artery embolization may be favourable in more stable patients (1-7). Both techniques infer risk of post-operative infection; abscess formation or decreased immunity to the patient though may prevent fatal hemorrhage. There is no gold standard therapy for SPH and future studies would benefit in investigating the benefit of treating SPH with medications such as beta-blockers and surgery, particularly in children or in those who have a history of hereditary pancreatitis causing chronic disease.
Acknowledgments
We thank the patient and his family for allowing us to share their information.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dx.doi.org/10.21037/pm-21-30
Peer Review File: Available at https://dx.doi.org/10.21037/pm-21-30
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/pm-21-30). AM reports that he received speaking honorarium from Terumo, Boston Scientific, Medtronic and Teleflex, and participated in a medical advisory board for Boston Scientific. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s substitute decision maker for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cakmak O, Parildar M, Oran I, et al. Sinistral portal hypertension; imaging findings and endovascular therapy. Abdom Imaging 2005;30:208-13. [Crossref] [PubMed]
- Sakorafas GH, Tsiotou AG. Splenic-vein thrombosis complicating chronic pancreatitis. Scand J Gastroenterol 1999;34:1171-7. [Crossref] [PubMed]
- Wang L, Liu GJ, Chen YX, et al. Sinistral portal hypertension: clinical features and surgical treatment of chronic splenic vein occlusion. Med Princ Pract 2012;21:20-3. [Crossref] [PubMed]
- Madsen MS, Petersen TH, Sommer H. Segmental portal hypertension. Ann Surg 1986;204:72-7. [Crossref] [PubMed]
- Little AG, Moossa AR. Gastrointestinal hemorrhage from left-sided portal hypertension. An unappreciated complication of pancreatitis. Am J Surg 1981;141:153-8. [Crossref] [PubMed]
- Liu Q, Song Y, Xu X, et al. Management of bleeding gastric varices in patients with sinistral portal hypertension. Dig Dis Sci 2014;59:1625-9. [Crossref] [PubMed]
- Tang SH, Zeng WZ, He QW, et al. Repeated pancreatitis-induced splenic vein thrombosis leads to intractable gastric variceal bleeding: A case report and review. World J Clin Cases 2015;3:920-5. [Crossref] [PubMed]
- Sunakawa H, Tokuhara D, Yamamoto A, et al. Successful emergency combined therapy with partial splenic arterial embolization and endoscopic injection therapy against a bleeding duodenal varix in a child. Clin J Gastroenterol 2015;8:138-42. [Crossref] [PubMed]
- Kiani MA, Forouzan A, Masoumi K, et al. Isolated Splenic Vein Thrombosis: 8-Year-Old Boy with Massive Upper Gastrointestinal Bleeding and Hypersplenism. Case Rep Pediatr 2015;2015:480507. [Crossref] [PubMed]
- McElroy R, Christiansen PA. Hereditary pancreatitis in a kinship associated with portal vein thrombosis. Am J Med 1972;52:228-41. [Crossref] [PubMed]
Cite this article as: Bortolin KA, Jones SA, Mujoomdar A, Zizzo AN. A sinister source of gastrointestinal bleeding treated by transhepatic splenic varix embolization in a paediatric patient: a case report. Pediatr Med 2021;4:39.