
National Very Preterm Infant Register imbedded in the Medical Birth Register in Finland
Background information
Finland is a Northern European country with approximately 5.5 million inhabitants and an area of approximately 338,000 square kilometers. The annual number of births has declined over the past decade, from around 60,000 in 2010 to 45,000 in 2019 (1). The rate of preterm deliveries (before 37 gestational weeks) has been stable at 5.5–6.0% over the last decade. Neonatal and infant mortality rates have been 1.2 and 1.7 per 1,000 live births, respectively, which is low in international comparison (2). There are five tertiary neonatal intensive care units (NICUs), affiliated with the university hospitals, in Finland. The number of other delivery hospitals has been brought down from 33 hospitals in 2002 to 18 in 2020. The rate of very preterm deliveries (before 32 gestational weeks) has also remained steady at 0.7–0.8%. The survival rate of very preterm infants (gestational age 24+0 to 29+6 weeks) was 88.1% during 2007–2013 (3). Care practices for very preterm infants comply with current evidence-based science (4) indicated by the following examples; 90–95% of very preterm infants are born in the five tertiary hospitals of the country (5), over 90% are exposed to antenatal corticosteroids (3) and early nasal continuous positive airway pressure is in frequent use.
The Finnish Medical Birth Register (FinMBR) (6) has collected data on all newborn infants in Finland since 1987 in order to develop and organize maternity care, obstetrical services and neonatal care. It includes detailed data on all pregnancies, births, newborn infants and the early neonatal period. The data on pregnancies include maternal demographic background factors and pregnancy history, antenatal follow-up visits, mother’s weight and height, smoking, other risk factors and interventions, diseases and hospital care during pregnancy. The data on births include the place of birth, gestational age at the time of delivery, mode and duration of the delivery, pain management and procedures during delivery, and diagnoses relating to pregnancy and delivery. The data on newborn infants include sex, growth measurements, Apgar scores and umbilical pH, information on common care interventions, any ICD-10 diagnoses and hospital care, and survival status by the age of 7 days. In addition, the length of stay in hospital is collected for the mother. The data collection form has been modified in 1990, 1996, 2004 and 2017 to better meet clinical needs. An exhaustive list of currently included variables can be found on the associated website (7).
FinMBR is owned by the Finnish Institute for Health and Welfare (THL), which operates under the Ministry of Social Affairs and Health. Its power is its legal position as a statistical authority: it can mandate public and private hospitals to provide information. All delivery hospitals in Finland are public hospitals. The register covers nearly 100% of pregnancies and newborns, including all live births and stillborn fetuses with a birth weight of at least 500 g or with a gestational age of at least 22 weeks. Planned home births are rare and assisting health care personnel are obligated to submit the birth information to FinMBR. In the case of unplanned home birth or birth en route to a hospital, the unit admitting and eventually discharging the infant submits the register data. The register is linked to the Central Population Register kept by the Digital and Population Data Services Agency to identify unreported live births and to the Cause-of-Death Register to identify unreported stillbirths and infant deaths. The annual number of live births has ranged from 45,753 in 2019 to 66,642 in 1992. This number has differed from the Central Population Register by 0.0% to 1.2%, since the FinMBR includes also births by temporary residents, recent migrants and visitors. Missing data entries are queried by the FinMBR staff. The register is allowed to collect data on newborns until discharge or up to seven days. The FinMBR data has been shown to have high validity (8). The register is also used to complete other registers, for example all anomalies detected at any point during the initial postnatal hospitalization and reported to FinMBR are sent automatically to the Register of Congenital Malformations, and all major congenital anomalies are included in their data after validation.
Development of the Finnish Very Preterm Infant Register
There was a clear need to collect more detailed data on very preterm infants for quality comparison and quality improvement purposes. Two research projects paved the way for a national register for very preterm infants. One research project collected data on all infants born below 1000g in Finland during years 1996–1997 and 1999–2000 (9). Another, larger national research project, the PERFECT Preterm Infant Study (Performance, Effectiveness and Cost of Treatment Episodes), focused on regional and hospital-level (level 2 vs. level 3) performances (10-14) and cost-effectiveness (15-18) in the care of very preterm infants. The PERFECT Preterm Infant study was started in 2004 and utilized data from the Medical Birth Register and Hospital Discharge Register (later Care Register for Health Care) (19). The PERFECT study included infants who were born below 32 gestational weeks or below 1,501 g from 2000 through 2003. The study was done in collaboration with the Finnish Institute of Health and Welfare and all five University Hospitals in Finland. The PERFECT Preterm Infant Study was expanded to a European EuroHOPE study covering very preterm infants born in seven European countries born between 2006 and 2008 (20).
The Very Preterm Infant Register, a separate data collection within the Medical Birth Register and similarly owned by THL, was initiated in November 2004, collecting data on all infants born below 32+0 gestational weeks or with a birth weight below 1,501 g. All units caring for such infants are mandated to submit a large dataset covering the care of the infant until discharge or 42 weeks of postmenstrual age, whichever comes first. An exhaustive list of currently included variables can be found on the associated website (7).
Leading neonatologists from all university hospitals planned the items to be collected, together with experts from THL. Over 100 data items were included covering pregnancy, delivery and neonatal treatments, nutrition, examinations, and any ICD-10 diagnoses. In addition, the survival status, growth measurements, and type of feeding are requested at 42 weeks of postmenstrual age or discharge. The follow up until 42 weeks of postmenstrual age corresponds to the developmental age of full-term infants at the time of their data submission. When considering the included population, it was regarded important to include also infants born in level 1 and level 2 hospitals during those years to be able to monitor the safety of this practice. The cases reported to the Very Preterm Infant Register are linked to the FinMBR to complete the data and to identify any missing cases. Birth hospitals and the hospitals responsible for neonatal care episodes of very preterm infants are requested to retrospectively complete any missing information or missing cases.
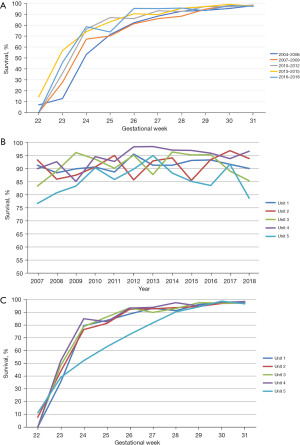
The register keeper, THL, has been responsible for organizing meetings to discuss the register development and utilization with clinicians. A group of leading neonatologists from the five university hospitals has been active in providing feedback, and subsequently the data collection forms have been amended as needed. A significant structural development occurred in 2018, when the web-based “data cube” interface was created, which enables clinicians to compare data in the Very Preterm Infant Register with filters such as gestational age, birth hospitals or time periods for comparisons of the whole variety of collected variables. Graphs enable yearly time trends throughout the register period from 2007 or clustered 3-year cohorts, which smooth case-mix variation in small patient populations. Figure 1A-1C demonstrate examples of data display options, which show the national improvement in survival rates and the variation in survival of very preterm/very low birth weight infants in the five level 3 neonatal intensive care units in Finland. The denominator used in these graphs are all live-born infants, and the outcome of survival is defined as survival to one year after birth. The low survival among infants born at 22 gestational weeks reflects the care practice at the limits of viability, where the initiation of active care is decided individually based on background factors and parental preference.
The mission of this register is to provide data for quality improvement purposes. Finland is preparing its first legislation on health care quality registers in 2021, and it would be desirable to include also the Very Preterm Infant Register as an official health care quality register.
Network activities
Research activity laid the basis for the Very Preterm Infant Register within the FinMBR, which then has enabled further research activity. A number of studies have been performed utilizing the Very Preterm Infant Register. The themes studied include the centralization of very preterm deliveries (5,21); the epidemiology of prematurity (22-24); specific patient groups such as cancer survivors (25,26); and the exposure to antenatal steroids (27). The Very Preterm Data Register has been used as a part of the large International Network for Evaluating Outcomes in Neonates (iNeo) research collaboration. The Very Preterm Data file data have also been used in the European research collaborations, such as RECAP (Research on European Children and Adults born Preterm) (28) and Euro-Peristat on perinatal health information systems (29). The Nordic Medical Birth Registers have collaborated for a long time for research (30) and statistics compiled and published by THL every second year (31).
Engagement activities for participating members
The main purpose of the data collection on very preterm infants is to improve the quality of care in this patient group in Finland. When the data is completed and checked, it is shared with the university hospital neonatologists, and their teams at their discretion, who can reach the data using a password granted from the THL. For confidentiality reasons, the data cannot be published openly, but the routine reporting includes information on prematurity. Summaries of the data have been presented in national perinatal and pediatric conferences. In addition, clinicians discuss the data locally and nationally. These discussions feedback to the THL for improvements in the data collection and reporting.
At the time when the Very Preterm Infant Register was started, large differences could be seen in the care approaches between the university hospitals. Many care practices became more uniform quite quickly after the differences became visible. For example, the large variation in the length of stay between the hospitals disappeared and the use of surfactant became uniform for infants born at 23 weeks indicating a consistent, active approach to their care. These changes, among others, can be seen as a positive result of collecting and sharing the data.
Challenges and future directions
The step to implement data cubes was important to make the data much more useful; the data cubes enabled more specific questions to be asked and answered with the data. However, any omissions or errors in the data may lead to large deviations in the data because of small numbers; the population of Finland is only approximately 5.5 million and the rate of preterm birth (before 37 gestational weeks) is low (5.5% in 2019). This calls for knowledge of the local data, double checking and caution in interpretations. The risk for mistakes or misinterpretations has to be balanced with openness and dissemination of the data. At this point, the dissemination is compromised for data safety and confidentiality. Wider dissemination of the data in multiprofessional societies would, however, be important to improve expert engagement in quality improvement. We are continuously collaborating among the five university hospitals using the data cubes to tease out potential differences between unit practices and outcomes. Benchmarking visits have been done earlier; the continuous data will provide units with inferior outcomes an opportunity to identify potential better-performing benchmarking sites, e.g., regarding respiratory management, infection control or brain outcomes.
There is a need to automatize the data transfer, which now is done manually. The current process is laborious and prone to errors. Current information technology should be able to transfer clinical data to a register without manual work. The long-term vision is that electronical medical health records could be used as the primary source of register data.
The goal of the care of preterm infants is a healthy child who can cope with the challenges in school and social life. To develop care in the right direction, we should evaluate the desired final outcome. In order to do this, we need linkage to registers including long-term diagnoses, child development, and school performance. Currently data linkages are feasible for example with the primary health care register including data on children’s height and weight, medication, treatment in specialized care and social reimbursements for example for rehabilitation and disability benefits. In the optimal situation, we would perform a standardized test for all very preterm infants at a standardized age point to be collected and registered in the Very Preterm Infant Register. Information from parents could also be collected by using mobile phone applications, which can include standardized questionnaires. Digital solutions such as the above mentioned are currently under-used in Finland and carry significant potential for future development.
Acknowledgments
The authors wish to acknowledge former and current leading neonatologists and Medical Birth Register personnel involved in the development and continuous improving efforts of the Very Preterm Infant Register: Sture Andersson, Marjo Metsäranta, Viena Tommiska, Samuli Rautava, Mikko Hallman, Timo Saarela, Outi Tammela, Ulla Sankilampi, Unto Häkkinen, Mikko Peltola, Eija Vuori, Anna Heino, Jouni Meriläinen and Sirkka Kiuru
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Shoo Lee and Prakesh Shah) for the series “Neonatal Networks for Outcomes Improvement: Evolution, Progress and Future” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://pm.amegroups.com/article/view/10.21037/pm-21-63/coif). The series “Neonatal Networks for Outcomes Improvement: Evolution, Progress and Future” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Database reporting - THL. [cited 2021 Oct 4]. Available online: https://thl.fi/en/web/thlfi-en/statistics-and-data/statistics-by-topic/database-reporting#Sexual%20and%20reproductive%20health
- European Perinatal Health Report 2015 - Euro-Peristat. [cited 2019 Nov 14]. Available online: https://www.europeristat.com/index.php/reports/european-perinatal-health-report-2015.html
- Helenius K, Sjörs G, Shah PS, et al. Survival in Very Preterm Infants: An International Comparison of 10 National Neonatal Networks. Pediatrics 2017;140:e20171264. [Crossref] [PubMed]
- Zeitlin J, Manktelow BN, Piedvache A, et al. Use of evidence based practices to improve survival without severe morbidity for very preterm infants: results from the EPICE population based cohort. BMJ 2016;354:i2976. [Crossref] [PubMed]
- Helenius K, Gissler M, Lehtonen L. Trends in centralization of very preterm deliveries and neonatal survival in Finland in 1987-2017. Transl Pediatr 2019;8:227-32. [Crossref] [PubMed]
- Parturients, deliveries and births - THL. [cited 2021 May 29]. Available online: https://www.thl.fi/en/web/thlfi-en/statistics/statistics-by-topic/sexual-and-reproductive-health/parturients-deliveries-and-births
- Medical Birth Register - THL. [cited 2021 Oct 4]. Available online: https://thl.fi/en/web/thlfi-en/statistics-and-data/data-and-services/register-descriptions/newborns#Data content of the Medical Birth Register
- Gissler M, Teperi J, Hemminki E, et al. Data quality after restructuring a national medical registry. Scand J Soc Med 1995;23:75-80. [Crossref] [PubMed]
- Tommiska V, Heinonen K, Lehtonen L, et al. No improvement in outcome of nationwide extremely low birth weight infant populations between 1996-1997 and 1999-2000. Pediatrics 2007;119:29-36. [Crossref] [PubMed]
- Rautava L, Lehtonen L, Peltola M, et al. The effect of birth in secondary- or tertiary-level hospitals in Finland on mortality in very preterm infants: a birth-register study. Pediatrics 2007;119:e257-63. [Crossref] [PubMed]
- Rautava L, Häkkinen U, Korvenranta E, et al. Health-related quality of life in 5-year-old very low birth weight infants. J Pediatr 2009;155:338-43.e1-3.
- Rautava L, Andersson S, Gissler M, et al. Development and behaviour of 5-year-old very low birthweight infants. Eur Child Adolesc Psychiatry 2010;19:669-77. [Crossref] [PubMed]
- Rautava L, Häkkinen U, Korvenranta E, et al. Health and the use of health care services in 5-year-old very-low-birth-weight infants. Acta Paediatr 2010;99:1073-9. [Crossref] [PubMed]
- Rautava L, Eskelinen J, Häkkinen U, et al. 5-year morbidity among very preterm infants in relation to level of hospital care. JAMA Pediatr 2013;167:40-6. [Crossref] [PubMed]
- Korvenranta E, Linna M, Häkkinen U, et al. Differences in the length of initial hospital stay in very preterm infants. Acta Paediatr 2007;96:1416-20. [Crossref] [PubMed]
- Korvenranta E, Lehtonen L, Peltola M, et al. Morbidities and hospital resource use during the first 3 years of life among very preterm infants. Pediatrics 2009;124:128-34. [Crossref] [PubMed]
- Korvenranta E, Linna M, Rautava L, et al. Hospital costs and quality of life during 4 years after very preterm birth. Arch Pediatr Adolesc Med 2010;164:657-63. [Crossref] [PubMed]
- Korvenranta E, Lehtonen L, Rautava L, et al. Impact of very preterm birth on health care costs at five years of age. Pediatrics 2010;125:e1109-14. [Crossref] [PubMed]
- Lehtonen L, Rautava L, Korvenranta E, et al. PERFECT preterm infant study. Ann Med 2011;43:S47-53. [Crossref] [PubMed]
- Numerato D, Fattore G, Tediosi F, et al. Mortality and Length of Stay of Very Low Birth Weight and Very Preterm Infants: A EuroHOPE Study. PLoS One 2015;10:e0131685. [Crossref] [PubMed]
- Helenius K, Helle E, Lehtonen L. Amount of Antenatal Care Days in a Context of Effective Regionalization of Very Preterm Deliveries. J Pediatr 2016;169:81-6. [Crossref] [PubMed]
- Jakobsson M, Gissler M, Paavonen J, et al. The incidence of preterm deliveries decreases in Finland. BJOG 2008;115:38-43. [Crossref] [PubMed]
- Räisänen S, Gissler M, Saari J, et al. Contribution of risk factors to extremely, very and moderately preterm births - register-based analysis of 1,390,742 singleton births. PLoS One 2013;8:e60660. [Crossref] [PubMed]
- Alenius S, Kajantie E, Sund R, et al. The Missing Siblings of Infants Born Preterm. Pediatrics 2018;141:e20171354. [Crossref] [PubMed]
- Madanat-Harjuoja LM, Malila N, Lähteenmäki PM, et al. Preterm delivery among female survivors of childhood, adolescent and young adulthood cancer. Int J Cancer 2010;127:1669-79. [Crossref] [PubMed]
- Melin J, Heinävaara S, Malila N, et al. Risk factors for preterm delivery among early onset cancer survivors: A Finnish register-based study. Int J Cancer 2019;144:1954-61. [Crossref] [PubMed]
- Räikkönen K, Gissler M, Kajantie E. Associations Between Maternal Antenatal Corticosteroid Treatment and Mental and Behavioral Disorders in Children. JAMA 2020;323:1924-33. [Crossref] [PubMed]
- Project Summary - RECAP preterm. [cited 2021 May 29]. Available online: https://recap-preterm.eu/about-recap-preterm/project-summary/
- Why Monitor Perinatal Health - Euro-Peristat. [cited 2021 May 29]. Available online: https://www.europeristat.com/index.php/our-project/why-monitor-perinatal-health.html
- Langhoff-Roos J, Krebs L, Klungsøyr K, et al. The Nordic medical birth registers--a potential goldmine for clinical research. Acta Obstet Gynecol Scand 2014;93:132-7. [Crossref] [PubMed]
- Perinatal statistics in the Nordic countries - THL. [cited 2021 May 29]. Available online: https://thl.fi/en/web/thlfi-en/statistics/information-on-statistics/quality-descriptions/perinatal-statistics-in-the-nordic-countries
Cite this article as: Lehtonen L, Helenius K, Gissler M. National Very Preterm Infant Register imbedded in the Medical Birth Register in Finland. Pediatr Med 2023;6:4.

