
The Canadian Neonatal Network: development, evolution, and progress
Background information
The term neonatal network refers to a group of neonatal intensive care units (NICUs) in different hospitals that participates in systematic data collection from infants based on a common protocol for the purposes of monitoring outcomes, quality improvement and research. The criteria for patient inclusion in a neonatal network database varies and most networks focus on the most vulnerable infants: typically, preterm infants born below 33 weeks’ gestation (1). The number of infants in this group is generally small for each NICU (30 to 200 per year) and most public health perinatal surveillance programs do not collect detailed clinical data that are necessary to support quality improvement activities e.g., use of antenatal steroids, respiratory management, or feeding strategies. Thus, neonatal networks play a key role in efforts to improve neonatal care and outcomes (2).
The Canadian Neonatal Network (CNN) was established in 1995 to monitor and evaluate changes in clinical practices and trends in neonatal outcomes in the setting of a publicly funded health care system. Canada has a population of 36 million people with ~360,000 annual births and is served by a publicly funded health care system in which individual provinces are responsible for planning and allocating most publicly insured health services. All hospitals are funded and managed by provincial governments, and the regionalization of perinatal care in each province has led to centralization of specialized maternity units and NICUs (3). Canadian NICUs are classified into 3 levels of care, with level 3 units providing intensive care, level 2 units providing intermediate care and level 1 units providing normal newborn care (4). Beginning with 16 level 3 NICUs in 1995, all 32 level 3 NICUs in Canada progressively joined the CNN in subsequent years (5). Over 105,000 annual births occur in hospitals with a level 3 NICU in Canada.
Network mission and structure
The mission of the CNN is “to be a network of Canadian researchers who conduct leading multidisciplinary, collaborative research dedicated to the improvement of neonatal-prenatal health and health care in Canada and internationally”. Specific goals of the CNN are: (I) to establish a national network of multidisciplinary Canadian researchers interested in neonatal-perinatal research; (II) to establish and maintain a truly national neonatal-perinatal database and provide the infrastructure to facilitate collaborative research; (III) to longitudinally study outcomes and variation in medical care that increases costs but does not improve outcomes; and (IV) to develop innovative research methods that can lead to improvements in health and quality of health care.
The CNN neonatal research network governance comprises a Governing Board, an Executive Committee, a coordinating centre, and participating sites (Figure 1), and a set of by-laws. The Governing Board is formed by seven senior clinician-scientists that have previously been involved in the CNN and sets the policies that allow the CNN to fulfill its mission statement and achieve its objectives. It is the final decision-making authority of the CNN and appoints the executive officers, including the Director and Associate Directors of the network. There are seven to nine executive officers that are appointed to five-year terms renewable once, and are responsible for executing the day-to-day operations and decision-making. The Executive Committee advises the Executive Officers on operational and management issues of the CNN and serves as the scientific review committee for research proposals. Executive Committee members are elected by CNN site members for 3-year terms renewable once.
Under the supervision of the Director, the coordinating centre is responsible for carrying out the daily activities of the CNN. These include project coordination, contract management, database management, software development, and data analysis. Additionally, subcommittees oversee specific activities, such as producing the Annual Benchmark Report and updating the database variables and definitions. In each participating site, the site investigator is responsible for coordinating data collection and participation in specific projects. Local data abstractors are responsible for data collection. Site participation is voluntary and member sites must commit to timely data collection and participation in network activities.
Network activities
Database
The CNN maintains a database designed to include data on infants admitted to participating sites for greater than or equal to 24 hours or those who died or were transferred to another level 2 or 3 facility within 24 hours. Infants admitted less than 24 hours are excluded from data collection since most are admitted for short observation periods and overall correspond to less than 2% of patient days in level 3 NICUs (2). The database serves as a platform for most of the CNN’s activities: benchmarking reports, outcomes research, quality improvement, clinical trials, training and mentoring, and advocacy and policy development. The database has been used in over 300 peer-reviewed publications (www.canadianneonatalnetwork.org).
The CNN provides standardized training for all dedicated site data abstractors (usually 1 or 2 per site), who follow a standard data dictionary and data collection protocol (6). Patient charts are retrospectively reviewed. The CNN developed and regularly updates the data-entry program which is installed in each site. The anonymized patient data are then entered electronically into a program that has built-in error checks at the point of entry. At the coordinating centre, uploaded data are cleaned and checked for completeness and accuracy, and potential errors are rechecked by participating sites. The CNN database has demonstrated high reliability and internal consistency (7). Data sharing agreements and waivers of individual informed consent from the relevant institutional ethics or quality improvement committees were obtained for each participating site and are updated annually. At each site, data are stored in a secured database located either on-site or in an alternate, secured off-site location (e.g., health records department or computer services department). In accordance with privacy laws in Canada, patient identifiers are stripped and replaced by anonymous, unique identifiers before data are transferred to the coordinating centre. Patient confidentiality is strictly observed at every stage. The final database is stored in a secured server on-site, with off-site backup. Data analysis and new projects must undergo review and approval from the CNN Executive Committee and from the Research and Ethics Board of the investigator leading the project.
Since its first version, the CNN database has changed significantly. Data fields have been added and definitions updated in order to adapt to changes in care practices and outcome definitions. For example, variables reflecting neonatal asphyxia and therapeutic hypothermia as well as magnetic resonance imaging results for infants with asphyxia were added in the past years as this became a standard of care. The latest CNN manual of definitions and data collection is available at our website (www.canadianneonatalnetwork.org).
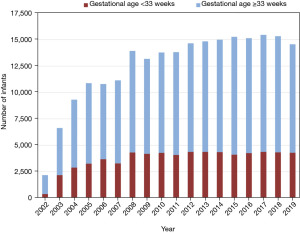
As the number of participating sites in the CNN grew, the number of infants included in the database increased steadily, reaching approximately ~15,000 infants per year in 2021 (Figure 2). All 32 participating sites currently collect data on eligible preterm infants born at <33 weeks’ gestation. In total, approximatively 4,400 infants per year born at <33 weeks’ are included in the database; this corresponds to approximately 85% of eligible infants in Canada since some infants born at ≥30 weeks are admitted directly in certain Level 2 NICUs (Figure 3). In addition to infants born at <33 weeks’ gestation, a majority of sites (~75%) also collect data on all other admissions born at ≥33 weeks, whereas other sites (~25%) report data on select groups of patients (e.g., infants with hypoxic ischemic encephalopathy or infants with major congenital anomalies). Additionally, 29 of the 30 sites with maternity services (2 sites in Canada have exclusive outborn populations) collect data on delivery room deaths of all infants born alive at ≥22 weeks’.

Benchmarking: annual report and web portal
Since its foundation, the CNN has produced regular annual reports, which allow individual sites to compare themselves to others in Canada. The report focuses mainly on outcomes of high-risk infants born at <33 weeks’ and <29 weeks’ gestation, evaluating care practices, resource use, and outcomes. The first CNN Annual Report reported the validation of a newborn severity score [Score for Acute Neonatal Physiology (SNAPII)] (8), a severity of illness scale [Neonatal Therapeutic Intervention Scoring System (NTISS)] (9), and an instrument for assessing infant transport outcomes [Transport Risk Index of Physiologic Stability (TRIPS)] (10). Including these 3 scores permitted the evaluation of risk-adjusted variations in mortality and morbidity among Canadian NICUs, and they are still used today as part of the CNN risk adjustment model (11-13).
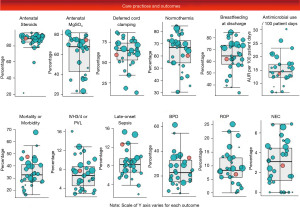
The annual report allows sites to evaluate the effects of local changes on site outcomes and how these compare to the rest of the country, but it is based on data from the previous year. The CNN also introduced a Semi-annual Quality Improvement Report on select morbidity trends for each site that provides more timely data (based on previous 6-month period) to better support quality improvement projects (www.canadianneonatalnetwork.org). We have since developed a web-based portal (using Microsoft ASP) that allows the application of multiple filters to visualize data in real time. Currently, the Annual Report continues to provide risk-adjusted analyses, while the web-based portal provides descriptive trends for each site and the entire network in real time.
Outcomes research
The goals of outcomes research are to identify and explain variations in care practices and outcomes and assess the effects of clinical care in a “real-life” setting (14). These are critical to improving neonatal care for several reasons. First, understanding how variations in practices correlate with variations in outcomes between countries, regions, and NICUs is a critical step in quality improvement and help identify better practices (15). Second, even when interventions are based on well designed randomized controlled trials, additional studies using contemporary data are necessary due to ongoing changes in the outcomes of preterm infants (16). Third, because infants included in randomized trials can be systematically different from non-enrolled infants, the estimated benefits of evidence-based practices may differ between populations (17). Fourth, epidemiologic research can help identify benefits and harms of interventions when data from large trials are lacking (18,19).
The CNN first focused on understanding the variations in outcomes between sites in Canada and risk-adjustment methodology (5,10,20). Its research then progressively expanded into the areas of generating better evidence for retinopathy of prematurity screening practices optimize timing and number of exams (21), identifying care practices associated with better outcomes (22), and evaluating the effects of staffing patterns on NICU outcomes (23). Today, the CNN research program includes quality improvement research, epidemiologic trend analyses, international comparisons, and long-term outcomes research (24-28).
Quality improvement program
To address ongoing variations in outcomes between sites and lack of improvement in outcomes over time (29), the CNN launched the Evidence-based Practice for Improving Quality program (30) in 2003 to improve outcomes of infants born <33 weeks’ gestation who are at high risk of mortality and morbidity (31,32). The Evidence-based Practice for Improving Quality (EPIQ) program is a collaborative, multifaceted quality improvement approach that is adapted from the Promoting Action on Research Implementation in Health Services (PARiHS) framework (33) and combines iterative learning techniques using Plan-Do-Study-Act cycles of rapid change with a process to facilitate quality improvement using the following approaches: (I) benchmarking with a standardized database, (II) best practice consensus from the best available evidence, (III) engagement of front-line staff, and (IV) mutual learning through networking. EPIQ additionally uses institution-specific data to target practices with high attributable risk of adverse outcomes for intervention within that; this strategy minimizes the use of inefficient “shotgun” approaches for practice change and emphasizes changing individual behaviour and organizational culture as much as practice change. Each institution can prioritize interventions aimed to improve a specific outcome. Since 2003, there have been 4 main iterations of EPIQ, with each one building on lessons learned from the previous years. We have shown that the program is scientific, generalizable, and sustainable (30,34,35). This program has contributed to significant and sustained improvements in the outcomes of preterm infants in Canada (25,36).
Health services and policy research
Health services research aims to improve the efficiency and effectiveness of the health care system (37). Improving perinatal care involves evaluation and planning for adequate resources, including NICU beds and human resources. In Canada, provinces are responsible for planning and allocating most publicly insured health services, leading to variations in resource allocation and health care delivery models (38). The CNN database, which includes details on infant trajectory of care (resource use, outcomes, discharge destination), provides valuable insights that aid the evaluation and planning of regional resources for neonatal care. Leveraging our database and expertise, the CNN has worked with several provinces to help identify regional needs related to NICU beds and human resources (39,40). Ongoing projects and partnerships with governments involve standardizing case-costing algorithms for neonatal care, prospective studies on human resource allocation, and developing standards for nurse-to-patient ratios in the NICU (41,42).
Development and linkage of sister networks
Since neonatal outcomes are dependent on a spectrum of care throughout the perinatal period, the CNN has expanded to incorporate and align its work with other perinatal activities. The Canadian Perinatal Network (CPN) was established to study and collect data on high-risk pregnancies in high risk maternity units across Canada. The Canadian Neonatal Follow-Up Network (CNFUN) collects standardized data on 18-month developmental outcomes of extremely preterm neonates born at <29 weeks’ gestation and admitted to CNN-participating NICUs from 26 neonatal follow-up programs across the country (26). Recognizing the increased rates of adverse outcomes for neonates not born in tertiary sites providing maternal-neonatal services (26), we helped to develop and link the Canadian Neonatal Transport Network (CNTN), which includes data on the transport of neonates from 16 specialized neonatal transport services in Canada (43). We also developed a close and linked partnership with the Canadian Pediatric Surgery Network (CAPSNet), which includes data on infants with gastroschisis and congenital diaphragmatic hernia treated in all 16 Canadian pediatric surgical hospitals in the country (44). A key element for the development of these sister networks was early collaboration with the CNN for harmonized variable definitions, data structure, data hosting and facilitated data linkage. Recently, we linked these networks and their databases and added antenatal variables under the umbrella of the Canadian Preterm Birth Network (CPTBN), which aims to create a flexible, transdisciplinary, evaluable, and informative research and quality-improvement platform focused on improving the outcomes of preterm infants (27).
Clinical trials
The CNN conducts clinical trials both directly and indirectly by providing an established infrastructure that facilitates site and patient recruitment, project coordination and data collection. Our first benchmark trial was a cluster-randomized trial evaluating the effects of a quality improvement program on the outcomes of preterm infants (34). This was followed by several other quality improvement trials, and trials evaluating the effectiveness of the Family Integrated Care model of care (30,45). In addition, the CNN provided support for other clinical trials by providing background data, information necessary to plan sample size, and information on site characteristics. In our next phase, we will leverage the network’s capabilities to engage as the “sole” platform for data collection for randomized controlled trials and to design the network database as a platform to identify and recruit patients for trials. Initial funded trials utilizing this platform includes the comparison of feeding strategy while receiving transfusion trial; and a cluster crossover trial on the resuscitation of preterm neonates with 30% and 60% oxygen.
Comparative effectiveness research (CER)
Comparative effectiveness trials compare existing health care interventions to identify which is more effective in improving patient outcomes (46). In the context of neonatal research, NICUs self-select to adopt a specific intervention or protocol and then patient outcomes of different interventions are compared using the CNN database. This allows the inclusion of all eligible infants in the NICUs, reduces trial costs, and leverages existing databases. The CNN is completing a CER project comparing bovine lipid surfactant extract and poractant alpha surfactant for preterm neonates born at <29 weeks’ gestation and is leading several other CER studies evaluating the effects of different strategies for non-invasive ventilation and patent ductus arteriosus management.
Training and mentoring
The CNN provides a solid platform for students, trainees, and junior investigators to learn research methods and execute projects (27). Trainees from multidisciplinary backgrounds benefit from the unique learning opportunities provided by the CNN. Trainees can either become involved via their local site investigators and submit project proposals or be hosted at the CNN coordinating centre while continuing formal research training in their local academic institution. The network encourages the use of its data for Master’s degree and PhD student projects.
Family support
In order to provide collaborative and mutual support on issues related to advocacy for parents and families of infants admitted to NICUs, the CNN has partnered with the Canadian Premature Babies Foundation (the national parent-led organization that aims to improve the parent experience in the NICU). In addition, several members of the Canadian Premature Babies Foundation serve as parent representatives on CNN research projects. The CNN also led the way in establishing and disseminating the concept of Family Integrated Care (FICare) both in Canada and internationally (30,45). FICare extends the concept of family integrated care by fully integrating families as partners in the NICU care teams; this has been shown to improve not only family satisfaction but also long-term neurodevelopmental outcomes of the infants (47).
International collaboration and training
International collaborations
Exploring regional differences in clinical management and outcomes plays a crucial part in improving neonatal care, and looking outward to other networks can be invaluable in this process. Collaborative research with other networks allows us to increase sample sizes for studies involving less frequent exposures and improve the generalizability of findings across different populations. The first population-based retrospective comparison, between Canada and Japan, showed that Japan had significantly lower rates of mortality, severe neurological injury, nosocomial infection, and necrotizing enterocolitis among very preterm infants, but higher rates of bronchopulmonary dysplasia and ≥ stage 3 retinopathy of prematurity; this led to both countries re-examining their practices in the relevant areas (48). CNN was instrumental in developing international collaborations, initially through the International Neonatal Collaboration (INC), and later through the International Network for Evaluating Outcomes of Neonates (iNeo), which was formed to facilitate international collaborative research for very low birth weight, very preterm infants (1). The iNeo platform (discussed in detail in another article in this series) is hosted at the CNN coordinating centre and collects data from 11 countries around the world on >15,000 neonates per year born <29 weeks’ gestation.
International training
The CNN established International Training Programs through collaborations with different universities and hospitals in China and India beginning in 2004. The objectives of these programs are to support the training of neonatologists and neonatal nurses using a ‘train the trainer’ approach, establish national standards for the training of neonatologists and neonatal nurses, and upgrade the standards of neonatal care and research. These training programs were developed by CNN members with expertise in medical education in collaboration with local institutions to address their specific needs. Systematic training is provided by CNN faculty both in the host countries and in Canada through teaching courses and mentorship and fellowship training programs.
Engagement activities for participating members
The CNN is committed to creating value for its members while striving to improve the outcomes of very preterm infants. In a large country like Canada, where sites are geographically distant from one another, creating a community is essential. We have used different methods to achieve this goal. First, the CNN Executive Committee is formed by investigators from different sites, allowing then to quickly address challenges that may be specific to certain areas in the country. Second, the web-based portal and Annual Report allows sites to stay engaged with one another in the process of quality improvement and identify local priorities for improvements (Figure 4). Third, the EPIQ program has multiple working groups aiming to improve specific outcomes (e.g., bronchopulmonary dysplasia, retinopathy of prematurity, necrotizing enterocolitis, brain injury, nosocomial infections). These groups coordinate multiple teleconferences each year where sites can share experiences and discuss the challenges and successes of their targeted quality improvement projects. Bundles of best practices can then be developed and disseminated to all members. Fourth, the CNN Annual Meeting allows site representatives to meet in person, share their experiences with quality improvement activities, and discuss ongoing and upcoming research collaborations. Fifth, to encourage the use of CNN data, all research proposals from the site investigators are supported (scientific review and data analysis) by the CNN coordinating centre. Finally, the CNN is in regular communication with its members, via teleconference, e-mail, newsletters, its official website and social media to provide updates, detail changes in the database and data dictionary, highlight publications, disseminate funding opportunities, and share new project ideas.
Funding support: sources and return on investments
The CNN coordinating centre and infrastructure are mainly funded via research grants from the Canadian Institutes of Health Research, for quality improvement research, clinical trials, and epidemiologic research; by the provincial governments, for health services research and analyses; and by Mount Sinai Hospital. The majority of the operational budget of the CNN coordinating center has historically been covered by overlapping research grants and the host institution. The individual participating sites provide funding and resources for local data collection and related activities. This funding structure creates a dual challenge for sustainability. First, part of the infrastructure is dependent on grant success rates. Second, local site investments are dependent on the local economic context and constantly need to be justified. To address these challenges, the CNN continuously works to provide added value and a return on investment to its site members.
Challenges: current and future
The financial sustainability of the CNN organization is an ongoing challenge and requires careful planning. This includes regular applications for funding from multiple sources, including federal and provincial granting agencies, hospitals, philanthropic entities, and governments. Keeping members engaged and connected requires constant adaptation and the integration of new technologies, such as the virtual platform. Another challenge is avoiding “change fatigue”, particularly in the context of quality improvement. Machine learning algorithms may help develop better prediction models for outcomes such as bronchopulmonary dysplasia which could help tailor bedside interventions such as the timing and dose of postnatal steroids. Integrating new technologies, like targeted ultrasound, ventilator devices, and methods to delivery surfactant, offer unique opportunities to continue to engage our community. The emergence of new technologies and therapies like regenerative medicine and artificial intelligence will open new horizons but also present new challenges in the future.
Future directions
As the field of neonatology changes, so must neonatal networks. The CNN database remains at the core of our activities and it is constantly updated to generate data on new practices. However, the community’s culture of change drives us forward. This includes expanding and merging the database with other population-based data to include all lower-risk infants born at ≥33 weeks’ gestation, and extending its activities into the areas of resource allocation and policy research. The experience gained in leading quality improvement projects has expanded the EPIQ methodology to new areas, such as level 2 NICUs and neonatal follow-up programs. We also aim to continue engaging in international collaborations with other neonatal networks and focus on long-term outcomes such as school-aged function and health status into adulthood. In summary, the CNN is an ever-changing organization built on a community of researchers, providers, and families who are all dedicated to improving the outcomes of neonates. However, the CNN’s most important contribution may be intangible and long-lasting: it has created a unique culture of trust, collaboration, and cooperation among health care professionals, researchers, administrators, and families that will benefit infants and their families for many generations to come.
Acknowledgments
The authors gratefully acknowledge all site investigators, abstractors, and trainers of the Canadian Neonatal Network (CNN). The lists of participating CNN site investigators and governing board members and their affiliations are provided below. We also thank Heather McDonald Kinkaid, PhD, a scientific writer at the Maternal-Infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada, for editorial support in preparing this manuscript; and other MiCare staff, for organizational and statistical support of CNN.
CNN investigators and affiliations: Prakesh S. Shah, MD, MSc (Director, Canadian Neonatal Network and Site Investigator), Mount Sinai Hospital, Toronto, Ontario; Marc Beltempo, MD (Associate Director, Canadian Neonatal Network and Site Investigator), Montreal Children’s Hospital at McGill University Health Centre, Montréal, Québec; Jaideep Kanungo, MD, Victoria General Hospital, Victoria, British Columbia; Joseph Ting, MD, British Columbia Women’s Hospital, Vancouver, British Columbia; Zenon Cieslak, MD, Royal Columbian Hospital, New Westminster, British Columbia; Rebecca Sherlock, MD, Surrey Memorial Hospital, Surrey, British Columbia; Ayman Abou Mehrem, MD, Foothills Medical Centre, Calgary, Alberta; Jennifer Toye, MD, and Khalid Aziz, MBBS, Royal Alexandra Hospital, Edmonton, Alberta; Carlos Fajardo, MD, Alberta Children’s Hospital, Calgary, Alberta; Jaya Bodani, MD, Regina General Hospital, Regina, Saskatchewan; Lannae Strueby, MD, Royal University Hospital, Saskatoon, Saskatchewan; Mary Seshia, MBChB, and Deepak Louis, MD, Winnipeg Health Sciences Centre, Winnipeg, Manitoba; Ruben Alvaro, MD, St. Boniface General Hospital, Winnipeg, Manitoba; Amit Mukerji, MD, Hamilton Health Sciences Centre, Hamilton, Ontario; Orlando Da Silva, MD, MSc, London Health Sciences Centre, London, Ontario; Sajit Augustine, MD, Windsor Regional Hospital, Windsor, Ontario; Kyong-Soon Lee, MD, MSc, Hospital for Sick Children, Toronto, Ontario; Eugene Ng, MD, Sunnybrook Health Sciences Centre, Toronto, Ontario; Brigitte Lemyre, MD, The Ottawa Hospital, Ottawa, Ontario; Thierry Daboval, MD, Children’s Hospital of Eastern Ontario, Ottawa, Ontario; Faiza Khurshid, MD, Kingston General Hospital, Kingston, Ontario; Victoria Bizgu, MD, Jewish General Hospital, Montréal, Québec; Keith Barrington, MBChB, Anie Lapoint, MD, and Guillaume Ethier, NNP, Hôpital Sainte-Justine, Montréal, Québec; Christine Drolet, MD, and Bruno Piedboeuf, MD, Centre Hospitalier Universitaire de Québec, Sainte Foy, Québec; Martine Claveau, MSc, LLM, NNP, Montreal Children’s Hospital at McGill University Health Centre, Montréal, Québec; Marie St-Hilaire, MD, Hôpital Maisonneuve-Rosemont, Montréal, Québec; Valerie Bertelle, MD, and Edith Masse, MD, Centre Hospitalier Universitaire de Sherbrooke, Sherbrooke, Québec; Roderick Canning, MD, Moncton Hospital, Moncton, New Brunswick; Hala Makary, MD, Dr. Everett Chalmers Hospital, Fredericton, New Brunswick; Cecil Ojah, MBBS, and Luis Monterrosa, MD, Saint John Regional Hospital, Saint John, New Brunswick; Julie Emberley, MD, Janeway Children’s Health and Rehabilitation Centre, St. John’s, Newfoundland; Jehier Afifi, MB BCh, MSc, IWK Health Centre, Halifax, Nova Scotia; Andrzej Kajetanowicz, MD, Cape Breton Regional Hospital, Sydney, Nova Scotia; Shoo K. Lee, MBBS, PhD (Chairman, Canadian Neonatal Network), Mount Sinai Hospital, Toronto, Ontario.
CNN Governing board members and affiliations: Shoo K. Lee, MBBS, PhD (Chairman, Canadian Neonatal Network), Mount Sinai Hospital, Toronto, Ontario; Bruno Piedboeuf, MD (Vice-Chairman), Centre Hospitalier Universitaire de Québec, Sainte Foy, Québec; Khalid Aziz, MBBS, Royal Alexandra Hospital, Edmonton, Alberta; Douglas McMillan, MD, IWK Health Centre, Halifax, Nova Scotia; Nalini Singhal, MD, Foothills Hospital, Calgary, Alberta; Eugene Ng, MD, Sunnybrook Hospital, Toronto, Ontario; Anne Monique Nyut, MD, Hôpital Sainte-Justine, Montréal, Québec.
Funding: Although no specific funding was received for this study, organizational support for the Canadian Neonatal Network™ was provided by the Maternal-infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada. MiCare is supported by the Canadian Institutes of Health Research (CTP 87518) and Mount Sinai Hospital. The authors Beltempo, Shah, and Lee are supported and funded by the Canadian Institutes of Health Research (Canadian Preterm Birth Network Grant, PBN 150642).
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Pediatric Medicine for the series “Neonatal Networks for Outcomes Improvement: Evolution, Progress and Future”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (https://pm.amegroups.com/article/view/10.21037/pm-21-80/coif). The series “Neonatal Networks for Outcomes Improvement: Evolution, Progress and Future” was commissioned by the editorial office without any funding or sponsorship. PSS served as the unpaid Guest Editor of the series. SKL served as the unpaid Guest Editor of the series and serves as the unpaid editorial board member of Pediatric Medicine from September 2022 to August 2024. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shah PS, Lee SK, Lui K, et al. The International Network for Evaluating Outcomes of very low birth weight, very preterm neonates (iNeo): a protocol for collaborative comparisons of international health services for quality improvement in neonatal care. BMC Pediatr 2014;14:110. [Crossref] [PubMed]
- Beltempo M, Carson C, DaSilva O et al. The Canadian Neonatal Network 2019 Annual Report. 2020. Available online: http://www.canadianneonatalnetwork.org/portal/Portals/0/Annual%20Reports/2019%20CNN%20report%20final_links.pdf (Accessed June 18 2021)
- Beltempo M, Carson C, DaSilva O et al. The Canadian Neonatal Network 2017 Annual Report. 2018. Available online: http://www.canadianneonatalnetwork.org/portal/Portals/0/Annual%20Reports/2017%20CNN%20report%20final_amendment.pdf (Accessed June 18 2021)
- Rizzolo A, Shah PS, Bertelle V, et al. Association of timing of birth with mortality among preterm infants born in Canada. J Perinatol 2021;41:2597-606. [Crossref] [PubMed]
- Lee SK, McMillan DD, Ohlsson A, et al. Variations in practice and outcomes in the Canadian NICU network: 1996-1997. Pediatrics 2000;106:1070-9. [Crossref] [PubMed]
- The Canadian Neonatal Network. CNN Abstarctor's Manual v.2.1.2. Available online: http://www.canadianneonatalnetwork.org/portal/CNNHome/Publications.aspx2014 (Accessed June 18 2021)
- Shah PS, Seidlitz W, Chan P, et al. Internal Audit of the Canadian Neonatal Network Data Collection System. Am J Perinatol 2017;34:1241-9. [Crossref] [PubMed]
- Richardson DK, Corcoran JD, Escobar GJ, et al. SNAP-II and SNAPPE-II: Simplified newborn illness severity and mortality risk scores. J Pediatr 2001;138:92-100. [Crossref] [PubMed]
- Gray JE, Richardson DK, McCormick MC, et al. Neonatal therapeutic intervention scoring system: a therapy-based severity-of-illness index. Pediatrics 1992;90:561-7. [Crossref] [PubMed]
- Lee SK, Zupancic JA, Pendray M, et al. Transport risk index of physiologic stability: a practical system for assessing infant transport care. J Pediatr 2001;139:220-6. [Crossref] [PubMed]
- Zupancic JA, Richardson DK, Horbar JD, et al. Revalidation of the Score for Neonatal Acute Physiology in the Vermont Oxford Network. Pediatrics 2007;119:e156-63. [Crossref] [PubMed]
- Beltempo M, Shah PS, Ye XY, et al. SNAP-II for prediction of mortality and morbidity in extremely preterm infants. J Matern Fetal Neonatal Med 2019;32:2694-701. [Crossref] [PubMed]
- Lee SK, Aziz K, Dunn M, et al. Transport Risk Index of Physiologic Stability, version II (TRIPS-II): a simple and practical neonatal illness severity score. Am J Perinatol 2013;30:395-400. [PubMed]
- Jefford M, Stockler MR, Tattersall MH. Outcomes research: what is it and why does it matter? Intern Med J 2003;33:110-8. [Crossref] [PubMed]
- Rankin KM, Gavin L, Moran JW Jr, et al. Importance of Performance Measurement and MCH Epidemiology Leadership to Quality Improvement Initiatives at the National, State and Local Levels. Matern Child Health J 2016;20:2239-46. [Crossref] [PubMed]
- Stoll BJ, Hansen NI, Bell EF, et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. JAMA 2015;314:1039-51. [Crossref] [PubMed]
- Rich W, Finer NN, Gantz MG, et al. Enrollment of extremely low birth weight infants in a clinical research study may not be representative. Pediatrics 2012;129:480-4. [Crossref] [PubMed]
- Lodha A, Seshia M, McMillan DD, et al. Association of early caffeine administration and neonatal outcomes in very preterm neonates. JAMA Pediatr 2015;169:33-8. [Crossref] [PubMed]
- Lodha A, Shah PS, Soraisham AS, et al. Association of Deferred vs Immediate Cord Clamping With Severe Neurological Injury and Survival in Extremely Low-Gestational-Age Neonates. JAMA Netw Open 2019;2:e191286. [Crossref] [PubMed]
- Synnes AR, Chien LY, Peliowski A, et al. Variations in intraventricular hemorrhage incidence rates among Canadian neonatal intensive care units. J Pediatr 2001;138:525-31. [Crossref] [PubMed]
- Lee SK, Normand C, McMillan D, et al. Evidence for changing guidelines for routine screening for retinopathy of prematurity. Arch Pediatr Adolesc Med 2001;155:387-95. [Crossref] [PubMed]
- Grunau RE, Oberlander TF, Whitfield MF, et al. Demographic and therapeutic determinants of pain reactivity in very low birth weight neonates at 32 Weeks' postconceptional Age. Pediatrics 2001;107:105-12. [Crossref] [PubMed]
- Lee SK, Lee DS, Andrews WL, et al. Higher mortality rates among inborn infants admitted to neonatal intensive care units at night. J Pediatr 2003;143:592-7. [Crossref] [PubMed]
- Shah PS, Lui K, Sjörs G, et al. Neonatal Outcomes of Very Low Birth Weight and Very Preterm Neonates: An International Comparison. J Pediatr 2016;177:144-152.e6. [Crossref] [PubMed]
- Lee SK, Beltempo M, McMillan DD, et al. Outcomes and care practices for preterm infants born at less than 33 weeks’ gestation: a quality-improvement study. CMAJ 2020;192:E81. [Crossref] [PubMed]
- Synnes A, Luu TM, Moddemann D, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed 2017;102:F235-4. [Crossref] [PubMed]
- Shah PS, McDonald SD, Barrett J, et al. The Canadian Preterm Birth Network: a study protocol for improving outcomes for preterm infants and their families. CMAJ Open 2018;6:E44-9. [Crossref] [PubMed]
- Isayama T, Lee SK, Yang J, et al. Revisiting the Definition of Bronchopulmonary Dysplasia: Effect of Changing Panoply of Respiratory Support for Preterm Neonates. JAMA Pediatr 2017;171:271-9. [Crossref] [PubMed]
- Shah PS, Sankaran K, Aziz K, et al. Outcomes of preterm infants <29 weeks gestation over 10-year period in Canada: a cause for concern? J Perinatol 2012;32:132-8. [Crossref] [PubMed]
- Lee SK, Shah PS, Singhal N, et al. Association of a quality improvement program with neonatal outcomes in extremely preterm infants: a prospective cohort study. CMAJ 2014;186:E485-94. [Crossref] [PubMed]
- Rysavy MA, Li L, Bell EF, et al. Between-hospital variation in treatment and outcomes in extremely preterm infants. N Engl J Med 2015;372:1801-11. [Crossref] [PubMed]
- Shah PS, Ye XY, Synnes A, et al. Prediction of survival without morbidity for infants born at under 33 weeks gestational age: a user-friendly graphical tool. Arch Dis Child Fetal Neonatal Ed 2012;97:F110-5. [Crossref] [PubMed]
- Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care 1998;7:149-58. [Crossref] [PubMed]
- Lee SK, Aziz K, Singhal N, et al. Improving the quality of care for infants: a cluster randomized controlled trial. CMAJ 2009;181:469-76. [Crossref] [PubMed]
- Shah PS, Dunn M, Aziz K, et al. Sustained quality improvement in outcomes of preterm neonates of <29 weeks' gestational age: results from the Evidence-based Practice for Improving Quality Phase 3 (EPIQ-3). Can J Physiol Pharmacol 2019;97:213-21. [Crossref] [PubMed]
- Lui K, Vento M, Modi N, et al. Inter-center variability in neonatal outcomes of preterm infants: A longitudinal evaluation of 298 neonatal units in 11 countries. Semin Fetal Neonatal Med 2021;26:101196. [Crossref] [PubMed]
- Lohr KN, Steinwachs DM. Health services research: an evolving definition of the field. Health Serv Res 2002;37:7-9. [PubMed]
- Allin S. Does Equity in Healthcare Use Vary across Canadian Provinces? Healthc Policy 2008;3:83-99. [Crossref] [PubMed]
- Beltempo M. Rapport sur l’évaluation des besoins régionaux en néonatologie au Québec. Rapport produit pour le Ministère de la santé et des Services sociaux du Québec. Montreal, QC, Canada, April 2021.
- Lee S, Cardiff K, Stewart S, et al. Report on Teritiary Neonatal Care in Bristish Columbia. Vancouver, BC, Canada, April 2002.
- Rios JD, Shah PS, Beltempo M, et al. Costs of Neonatal Intensive Care for Canadian Infants with Preterm Birth. J Pediatr 2021;229:161-167.e12. [Crossref] [PubMed]
- Lemieux-Bourque C, Piedboeuf B, Gignac S, et al. Comparison of Three Nursing Workload Assessment Tools in the Neonatal Intensive Care Unit and Their Association with Outcomes of Very Preterm Infants. Am J Perinatol 2022;39:640-5. [Crossref] [PubMed]
- Lee KS. Neonatal transport metrics and quality improvement in a regional transport service. Transl Pediatr 2019;8:233-45. [Crossref] [PubMed]
- Puligandla PS, Skarsgard ED. The Canadian Pediatric Surgery Network Congenital Diaphragmatic Hernia Evidence Review Project: Developing national guidelines for care. Paediatr Child Health 2016;21:183-6. [Crossref] [PubMed]
- O'Brien K, Robson K, Bracht M, et al. Effectiveness of Family Integrated Care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. Lancet Child Adolesc Health 2018;2:245-54. [Crossref] [PubMed]
- Greenfield S, Rich E. Welcome to the Journal of Comparative Effectiveness Research. J Comp Eff Res 2012;1:1-3. [Crossref] [PubMed]
- Synnes AR, Petrie J, Grunau RE, et al. Family integrated care: very preterm neurodevelopmental outcomes at 18 months. Arch Dis Child Fetal Neonatal Ed 2022;107:76-81. [Crossref] [PubMed]
- Isayama T, Lee SK, Mori R, et al. Comparison of mortality and morbidity of very low birth weight infants between Canada and Japan. Pediatrics 2012;130:e957-65. [Crossref] [PubMed]
Cite this article as: Beltempo M, Shah PS, Lee SK; the Canadian Neonatal Network (CNN). The Canadian Neonatal Network: development, evolution, and progress. Pediatr Med 2023;6:18.


