
The Spanish Neonatal Network SEN1500: updated information
Introduction
Very low birth weight (VLBW) and very preterm (VPT) infants, born with <1,500 g or <32 weeks or gestational age (GA) at birth, respectively, represent the most important risk groups for perinatal and neonatal mortality and morbidity (1,2). According to the Spanish National Institute of Statistics (INE) during the first two decades of the present century, 369,000 to 520,000 children were born yearly in Spain. Approximately, 0.9% of them were VLBW infants. Out of these, between 2,100 to 3,100 were admitted yearly to neonatal units of the SEN1500 network. It is estimated that this group of infants consumes approximately two-thirds of the resources invested in neonatology in Spain (3,4). In recent decades, advances in perinatal care have contributed to a significant improvement in VLBW/VPT infants’ survival (5). Hence, the relative relevance for the Health Care Systems (HCS) represented by these groups of patients is expected to further increase. Neurodevelopmental follow-up programs for VLBW/VPT infants up to 24 months corrected age constitute the minimum required standard of care for all our Neonatal Units. Follow-up programs enable an early identification and intervention upon specific morbidities aiming to improve long-term clinical outcomes (6).
Traditionally, the relatively small number of patients admitted in most neonatal units hampered putting forward adequately powered epidemiological studies or even pooling enough data to monitor trends properly and benchmark outcomes. Already in the late 1980s, two American-based collaborative networks, the Neonatal Research Network funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Vermont Oxford Network pioneered the concept of neonatal database network. Then, over the mid and late 1990s and early 2000s, neonatal networks were established in Australia and New Zealand (ANZNN, 1994), Canada (CNN; 1995), Israel (INN, 1995), Switzerland (SNN 1995), Sweden (SNQ, 2001), Japan (NRNJ, 2003), and the United Kingdom (UKNC) among others. Later, some of these networks merged their databases to create The International Network for Evaluating Outcomes (iNeo, 2013) (7-11). In Spain, the SEN1500 was created through the joint efforts of a significant number of units under the umbrella of a national neonatal network (12). The development of the SEN1500 database was instrumental in quantifying and monitoring temporal trends regarding perinatal and neonatal mortality, morbidity rates, neurodevelopmental outcomes in survivors at 24 months corrected age, and the frequency of different therapeutic and diagnostic interventions.
Constitution and aims of the SEN1500 network
The SEN1500 Network was founded under the leadership of the former Spanish Society of Neonatology (SENeo) president Professor Manuel Moro (12). SENeo (formerly abbreviated as SEN) is a non-profit medical-scientific association of Spanish neonatologists constituted in 2002, according to the 22nd article of the Spanish Constitution. The Board of the SENeo, aware of the relevance of network databases for research and quality improvement, boosted the creation of a project that aimed to gather Spanish Neonatal Units under the denomination “Database of Newborns under 1500 grams: SEN1500”. This database was initially divided into three sections: (I) morbidity and mortality; (II) socioeconomic factors; and (III) neuropsychological development at 24 months corrected age. Current SEN1500 network missions include epidemiological and outcomes surveillance, benchmarking and quality improvement, and research promotion (Table 1).
Table 1
| To monitor the perinatal, neonatal, and follow-up outcomes at 24 months corrected age, the socioeconomic environment and the quality of care delivered to VLBW infants, and since 2019 to all very preterm infants, admitted to the participant units |
| To periodically produce detailed statistical reports for every unit with their own and pooled data, helping the units identifying their stronger points and areas for further improvement |
| To openly disseminate the pooled whole network data, serving as a benchmarking platform, enhancing collaboration, and working as an opportunity to share local experiences leading to improvement at a wider level |
| To promote and provide data for epidemiological research in perinatal and neonatal medicine, facilitate multicenter randomized clinical trials and national quality improvement initiatives |
VLBW, very low birth weight.
From the beginning, neonatal units from hospitals from all over the country joined SEN1500. Since its inception, a team of epidemiologists and neonatologists checked the quality of the data, performed the statistical analysis, and elaborated the SEN1500 Annual Report which was made open access to all neonatologists in Spain. The first annual report, published in 2002, included data from 55 neonatal Level II and III Units. Nowadays, annual reports include data from around 60 to 65 neonatal units across Spain. During the presidency of Prof. Josep Figueras [2011–2014] SEN1500 joined the International Network for Epidemiological Outcomes (iNeo) contributing to the generation of very valuable epidemiological studies, in collaboration with Prof. Adolfo Valls. Finally, Prof. Maximo Vento (2015–2019), promoted a fruitful joint venture of SEN1500 with NEOCOSUR (https://neocosur.org/neocosur/vista/index.php), a neonatal network of countries of the southern region of Latin America (Argentina, Chile, Paraguay, Peru, and Uruguay).
In 2021, SEN1500 embarked on a new project with TUPL™ (https://www.tupl.com/), a company with expertise in big data, to boost SEN1500 digital transformation. As of 2022, different processes will be automatic, including checking the data quality, statistical analysis, and producing and emailing individualized reports to the local and national coordinators. The algorithm has been designed to reduce the time it takes to reach conclusions from the data, as the results will be readily available within hours once the data collection time is over. Even more, a website-based tool, also using these algorithms, has been created too. This tool allows any local or national coordinator to analyze and compare data at any time, selecting the desired variables, metrics, and temporal framework (Figure S1).
Description of the SEN1500 database
SEN1500 is a national database that includes level II and level III neonatal units classified as per the Spanish Neonatal Society criteria (13). In brief, Level II units have staff and equipment to provide the necessary care for newborns ≥32 weeks GA or ≥1,500 g with no anticipation of urgent subspecialized care at birth. Level II units with more than 1,500 deliveries per year that have the capability to provide invasive respiratory support for a brief period are classified as level II B units. Level III units are adequately staffed and equipped to provide continuous vital support and appropriate care for newborns <32 weeks GA or <1,500 g. Level III units provide prolonged assisted ventilation, have quick access to a wide range of pediatric subspecialties and to imaging studies, including computed tomography (CT), magnetic resonance imaging (MRI), and echocardiography. Pediatric ophthalmology services with an organized program for monitoring, and treatment of retinopathy of prematurity should be available. Regional and National reference units are levels III B and C. Levels IIIB and C units must have a pediatric general surgery department ready to treat acute surgical complications of prematurity immediately and the ability to provide advanced respiratory support (high frequency ventilation and inhaled nitric oxide). Level III C units are located in centers with Cardiovascular and Neurosurgery departments. Level III B and C units must run neonatal transport programs and provide continuing education within their area of influence.
The average number of voluntarily participating units over the last years has ranged between 62 and 65 units (Figures 1,2). Most of these neonatal units are funded by the government but 5.5% are private centers. Also, a large proportion of them are university-affiliated centers. The Spanish HCS was founded by Spain’s General Healthcare Act in 1986 and guarantees universal coverage and free healthcare access to all Spanish citizens, regardless of their economic situation or participation in the social security network. The HCS is principally funded via the national income tax. The HCS was transferred to the government of the Spanish administrative regions (called Autonomous Communities) in 2002. Since then, the regional healthcare authorities have been responsible for harmonizing and optimizing health care access to the population, thus avoiding the concentration of health services in selected areas. Private healthcare insurance is voluntary, and it is possible to have both a private and a public health coverage. Around 20% of the population, especially in the bigger cities, has a private insurance; however, private enterprises subcontract some highly specialized services to the public sector.

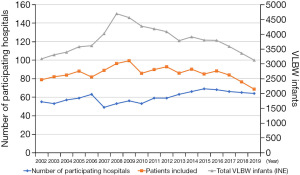
Currently, SEN1500 is a quasi-population-based network since it registers 68% of all VLBW infants born in Spain (Figure 2). Moreover, 82% of extremely low birthweight (ELBW) infants born in Spain are registered in SEN1500. The peak of admissions occurred in 2008–2009 and coincided with an overall increase of the birth rate in Spain (Figure S2).
Data collection (Figure 3)
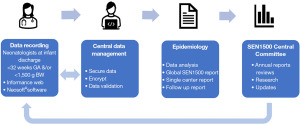
Data from newborns with a birthweight <1,500 grams have been systematically collected in the participating units. Since 2019, also newborns <32 weeks GA are included regardless of their birthweight. Data are collected using standardized definitions provided by the SEN1500 Operations Manual to assure homogeneity. The systematic and prospective gathering of these homogeneous indicators is key to timely monitoring of temporal outcome trends. It also enables inter-center comparisons to benchmark the quality of care delivered to VLBW/VPT infants within the network. Collected variables include sociodemographic features, perinatal care and morbidity and mortality up to first hospital discharge and thereafter until follow-up 24 months corrected age. The initial setlist of 140 variables is periodically updated, and new variables are added after discussion and agreement within the network’s steering committee every two years.
In each participating center, one or two neonatologists act as site coordinators. They are responsible for the patients’ registration, collecting and periodically submitting the de-identified and encrypted data electronically to the central database. The network coordinators verify the completion and consistency of the data and, if necessary, contact the local site coordinators should any doubt arise. The data analysis and representation are performed by a team of epidemiologists, and the national coordinators and database managers of the SEN1500 network.
Compliance with current regulations on data protection and funding
Data retrieval and registration in the SEN1500 follow the requirements of the Spanish and the International legislations as well as the local Ethics Committee requirements for Data Protection. At the site’s end, the local site coordinators guarantee the security of the data. At the network end, the centralized computing module has highly secure data custody and copy management that prevents data leaks and unauthorized access.
Participation in SEN1500 is voluntary. The use of SEN1500 data for research purposes is allowed for any of the participating centers upon request to the SEN1500 steering committee and the board of directors of the SENeo. In addition, SENeo’s budget runs with the maintenance costs of the database and central computer agency and the logistic support by the epidemiologists.
Scientific activity of the SEN1500 database
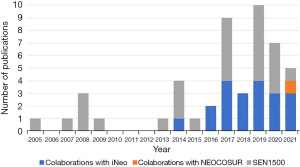
SEN1500 database has provided a unique opportunity for healthcare professionals, information technologies experts and health policymakers to participate in collaborative research projects on a national and international scale, suitable for publication in peer-reviewed journals (Figure 4). A list of published research studies is published yearly in the network reports and website (https://seneo.es).
All SENeo members are encouraged to use the database to conduct research studies. It is mandatory to fulfill an official request for data and address it to the SEN1500 steering committee, describing the purpose of the study to avoid duplications. Moreover, researchers are strictly committed to preserving the confidentiality of the patients and citing the origin of the data along with a list of the participating centers in the publications.
The first study carried out with data from the SEN1500 database was published in 2005 (14) and reported on the efficacy of prenatal corticosteroids in reducing mortality and chronic lung disease in premature infants between 23 and 28 weeks of GA.
Several articles published in national and international peer-review journals followed, adding up to a total of 48 articles by November 2021, counting on those produced in collaboration with other networks (Figure 4). They report on various aspects of neonatal epidemiology, such as in-hospital morbidity and mortality of VLBW/VPT infants and related factors, or the follow-up outcomes by two years (15,16), including the influence on neonatal morbidity and mortality of chorioamnionitis (17), a comparative study of outcomes between singletons and multiples (18), or the evaluation (19) and development (20) of predictive tools, among others. For instance, regarding chorioamnionitis, we found that its incidence was inversely related to GA at delivery, and, in VLBW infants ≤32 weeks’ GA, it was associated with higher risks of early-onset neonatal sepsis and necrotizing enterocolitis (NEC), but lower risks of patent ductus arteriosus (PDA) and late-onset neonatal sepsis, with no impact on mortality (17).
Most of the network-derived scientific data can be grouped into some specific topics. The first of these was the study of the limits of viability in our setting and related ethical aspects, which has been the subject of three studies (21-23). We showed that the proportion of survivors without major brain damage among survivors was relatively high and independent of the GA. These findings seemed to be related to end-of-life decisions and attitudes supporting the attitude of “giving an opportunity” even to the most immature patients when there was parental agreement.
Another important research area was related to nutrition, growth, and gastrointestinal morbidity, mainly NEC (24-32). In this set of works, we found that weight gain in the first weeks after birth is slow in extremely preterm infants and that there is an almost universal postnatal growth restriction that involves mainly length and weight (25,29), suggesting that a close control of longitudinal growth and head circumference are essential for nutritional assessment and detection of patients at risk for poor growth and neurodevelopment after hospital discharge. We concluded that some co-morbidities associated with prematurity have a special impact on postnatal growth. Female infants are at slightly higher risk of postnatal weight and head restriction after adjustment for morbidity (30). Regarding NEC, we described that its incidence remained stable over the last decade, but surgical treatment became more frequent in the last years while mortality decreased (31). We found that delayed cord clamping and extended access to donor milk were two possible aspects of further improvement in Spain. There were also inter-center variations in diagnostic and therapeutic aspects, most commonly in areas where evidence in the literature is weaker (32).
Respiratory morbidity and management have also been a matter of interest (14,33-35). We found that there has been an increased adherence of Spanish hospitals to the international recommendations in perinatal care during the past two decades. This was followed by a significant reduction in mortality, but survival without bronchopulmonary dysplasia (BPD) increased only among the most immature patients (33). In addition, we found great variability in clinical practice among Spanish centers and in the rates of survival and survival without BPD. Lower use of oxygen and less intubation in the delivery room were associated with an increased survival without BPD. In contrast, complications such as PDA, sepsis, and/or NEC were associated with a lower odds ratio of survival without BPD (34). More recently, we showed that despite increased use of non-invasive respiratory strategies, neither survival nor survival without moderate or severe BPD improved in VLBW infants under 32 weeks GA (35).
Finally, we also addressed aspects that may be key to optimizing resource allocation, finding a reduction of births during weekends and a clustering of high-risk births during this period, increasing the crude mortality and morbidity. However, differences disappeared after adjusting for confounding, suggesting an appropriate overall care in the centers (36). More recently, we showed that infants born during the night shift were more likely to be intubated at birth, receive surfactant, or develop anemia that required transfusion. Still there were no differences in survival rates or major morbidity (37).
Internationalization of the database SEN1500
The internationalization of SEN1500 has contributed enormously to expanding our scientific achievements and has allowed the global diffusion of the Spanish neonatology. Furthermore, it has made it possible to establish internetworks benchmarking studies aimed at detecting areas for improvement. Since its creation, some Spanish units collaborating with the SEN1500 network, also participated in EuroNeoNet (38), a project promoted by Prof. Adolfo Valls i Soler, consisting of a European information system on the outcomes of VLBW infants to monitor and improve the care of these infants throughout Europe. EuroNeoNet was founded in 2002 to ensure the best neonatal care possible for every VLBW infant cared for in Europe through standardized benchmarking, as well as promoting the safety of patients, the online training of health care professionals, and facilitating physician-initiated clinical trials. EuroNeoNet closed in 2015, but fortunately, a new platform, eNewborn, led by Professor Dominique Haumont, took over reviewing the data elements and integrating innovative information technology, original software, and international collaboration (39). The platform has recently moved from Brussels to Imperial College London, where it is now co-led by Professor Neena Mody. A SEN1500 collaboration project with eNewborn is underway, which we trust will become a reality in the coming months (40).
Apart from the aforementioned project, the two most relevant international collaborations so far, as mentioned above, have been with iNeo (41-60) and NEOCOSUR (61).
Conclusions
The Spanish SEN1500 database has just come of age. Since its origin and throughout its development, it has proven to be a fundamental tool for evaluating the quality of care for the very premature or VLBW newborns in the participating units, key to boosting sustained improvement. Participation in a national network allows individual centers, through a benchmarking process, to compare results and detect areas for improvement. It also allows knowing the individual and collective temporal evolution and planning multicenter studies. In addition, collaboration with other international networks has enhanced its ability to generate knowledge and has contributed to improving the quality of the SEN1500 network database itself. The evolution of information technologies and the possibility of massive data analysis require a permanent update of the computer sciences support tools and a renewed effort to maintain the quality of the data collected with due respect to the privacy of the patients and their families.
Acknowledgments
We would like to express our utmost gratitude to all the neonatologists who invested their time in introducing data to the SEN1500 database, thus providing researchers worldwide with an extremely valuable tool for improving the outcomes of our most vulnerable patients.
Funding: M.V. acknowledges Red de Salud Materno-Infantil y del Desarrollo (RETICS) funded by the PN 2018-2021 (Spain), ISCIII- Sub-Directorate General for Research Assessment and Promotion and the European Regional Development Fund (FEDER), reference RD16/0022. This study was supported by this project.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Shoo Lee and Prakesh Shah) for the series “Neonatal Networks for Outcomes Improvement: Evolution, Progress and Future” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://pm.amegroups.com/article/view/10.21037/pm-21-109/coif). The series “Neonatal Networks for Outcomes Improvement: Evolution, Progress and Future” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Patel RM, Kandefer S, Walsh MC, et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med 2015;372:331-40. [Crossref] [PubMed]
- Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 2015;385:430-40. [Crossref] [PubMed]
- Rogowski JA, Horbar JD, Plsek PE, et al. Economic implications of neonatal intensive care unit collaborative quality improvement. Pediatrics 2001;107:23-9. [Crossref] [PubMed]
- Rogowski J. Using economic information in a quality improvement collaborative. Pediatrics 2003;111:e411-8. [Crossref] [PubMed]
- Stoll BJ, Hansen NI, Bell EF, et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. JAMA 2015;314:1039-51. [Crossref] [PubMed]
- Pallás Alonso C, García González P, Jiménez Moya A, et al. Follow-up protocol for newborns of birthweight less than 1500 g or less than 32 weeks gestation. An Pediatr (Engl Ed) 2018;88:229.e1-229.e10.
- Lee SK, McMillan DD, Ohlsson A, et al. Variations in practice and outcomes in the Canadian NICU network: 1996-1997. Pediatrics 2000;106:1070-9. [Crossref] [PubMed]
- Donoghue DA, Cust AE. Australian and New Zealand Neonatal Network 1998. Sydney: AIHW National Perinatal Statistics Unit: Neonatal Network Series N.º 4, 2000.
- Horbar JD. The Vermont Oxford Network: evidence-based quality improvement for neonatology. Pediatrics 1999;103:350-9. [Crossref] [PubMed]
- Stevenson DK, Wright LL, Lemons JA, et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1993 through December 1994. Am J Obstet Gynecol 1998;179:1632-9. [Crossref] [PubMed]
- Shah PS, Lee SK, Lui K, et al. The International Network for Evaluating Outcomes of very low birth weight, very preterm neonates (iNeo): a protocol for collaborative comparisons of international health services for quality improvement in neonatal care. BMC Pediatr 2014;14:110. [Crossref] [PubMed]
- Moro Serrano M, Fernández Pérez C, Figueras Alloy J, et al. SEN1500: design and implementation of a registry of infants weighing less than 1,500 g at birth in Spain. An Pediatr (Barc) 2008;68:181-8. [Crossref] [PubMed]
- Rite Gracia S, Fernández Lorenzo JR, Echániz Urcelay I, et al. Health care levels and minimum recommendations for neonatal care. An Pediatr (Barc) 2013;79:51.e1-51.e11. [Crossref] [PubMed]
- Figueras-Aloy J, Serrano MM, Rodríguez JP, et al. Antenatal glucocorticoid treatment decreases mortality and chronic lung disease in survivors among 23- to 28-week gestational age preterm infants. Am J Perinatol 2005;22:441-8. [Crossref] [PubMed]
- Moro M, Pérez-Rodriguez J, Figueras-Aloy J, et al. Predischarge morbidities in extremely and very low-birth-weight infants in Spanish neonatal units. Am J Perinatol 2009;26:335-43. [Crossref] [PubMed]
- García P, San Feliciano L, Benito F, et al. Outcome at two years corrected age of a cohort of very low birth weight infants from hospitals within the neonatal SEN1500 network. An Pediatr (Barc) 2013;79:279-87. [PubMed]
- García-Muñoz Rodrigo F, Galán Henríquez G, Figueras Aloy J, et al. Outcomes of very-low-birth-weight infants exposed to maternal clinical chorioamnionitis: a multicentre study. Neonatology 2014;106:229-34. Erratum in: Neonatology 2015;107:42. [Crossref] [PubMed]
- Porta R, Capdevila E, Botet F, et al. Morbidity and mortality of very low birth weight multiples compared with singletons. J Matern Fetal Neonatal Med 2019;32:389-97. [Crossref] [PubMed]
- Guzmán Cabañas JM, Párraga Quiles MJ, et al. Usefulness of Clinical Risk Index for Babies based on birth weight in predicting hospital death and severe intraventicular hemorrhage in the SEN 1500 Spanish neonatal network. An Pediatr (Barc) 2009;71:117-27. [PubMed]
- Iriondo M, Thio M, Del Río R, et al. Prediction of mortality in very low birth weight neonates in Spain. PLoS One 2020;15:e0235794. [Crossref] [PubMed]
- García-Muñoz Rodrigo F, García-Alix Pérez A, García Hernández JA, et al. Morbidity and mortality in newborns at the limit of viability in Spain: a population-based study. An Pediatr (Barc) 2014;80:348-56. Erratum in: An Pediatr (Barc) 2015;82:121-3. [PubMed]
- García-Muñoz Rodrigo F, Díez Recinos AL, García-Alix Pérez A, et al. Changes in perinatal care and outcomes in newborns at the limit of viability in Spain: the EPI-SEN Study. Neonatology 2015;107:120-9. [Crossref] [PubMed]
- García-Muñoz Rodrigo F, Urquía Martí L, García Hernández JÁ, et al. End-of-Life Care and Survival without Major Brain Damage in Newborns at the Limit of Viability. Neonatology 2017;111:234-9. [Crossref] [PubMed]
- García-Muñoz Rodrigo F, García-Alix Pérez A, Figueras Aloy J, et al. New population curves in spanish extremely preterm neonates. An Pediatr (Barc) 2014;81:107-14. Erratum in: An Pediatr (Barc) 2015;82:122-3. [PubMed]
- Moreno Algarra MC, Fernández Romero V, Sánchez Tamayo T, et al. Variability in enteral feeding practices of preterm infants among hospitals in the SEN1500 Spanish neonatal network. An Pediatr (Barc) 2017;87:245-52. [Crossref] [PubMed]
- García-Muñoz Rodrigo F, Figueras Aloy J, Saavedra Santana P, et al. Postnatal growth at hospital discharge in extremely premature newborns in Spain. An Pediatr (Barc) 2017;87:301-10. [PubMed]
- Porta R, Capdevila E, Botet F, et al. Breastfeeding Disparities between Multiples and Singletons by NICU Discharge. Nutrients 2019;11:2191. [Crossref] [PubMed]
- Zozaya C, Avila-Alvarez A, Arruza L, et al. The Effect of Morbidity and Sex on Postnatal Growth of Very Preterm Infants: A Multicenter Cohort Study. Neonatology 2019;115:348-54. [Crossref] [PubMed]
- Zozaya C, Avila-Alvarez A, Couce ML, et al. Cohort study showed that growth rate increment has not been enough to prevent growth retardation of preterm infants and raised concerns about unbalanced growth. Acta Paediatr 2019;108:1793-800. [Crossref] [PubMed]
- Zozaya C, Avila-Alvarez A, García-Muñoz Rodrigo F, et al. The Impact of Postnatal Systemic Steroids on the Growth of Preterm Infants: A Multicenter Cohort Study. Nutrients 2019;11:2729. [Crossref] [PubMed]
- Zozaya C, García González I, Avila-Alvarez A, et al. Incidence, Treatment, and Outcome Trends of Necrotizing Enterocolitis in Preterm Infants: A Multicenter Cohort Study. Front Pediatr 2020;8:188. [Crossref] [PubMed]
- Zozaya C, Avila-Alvarez A, Somoza Argibay I, et al. Prevention, diagnosis and treatment of necrotising enterocolitis in newborns less than 32 weeks at birth in Spain. An Pediatr (Engl Ed) 2020;93:161-9.
- García-Muñoz Rodrigo F, Losada Martínez A, Elorza Fernández MD, et al. The Burden of Respiratory Disease in Very-Low-Birth-Weight Infants: Changes in Perinatal Care and Outcomes in a Decade in Spain. Neonatology 2017;112:30-9. [Crossref] [PubMed]
- García-Muñoz Rodrigo F, Urquía Martí L, Galán Henríquez G, et al. Intercenter variability and factors associated with survival without bronchopulmonary dysplasia in extremely preterm newborns. J Matern Fetal Neonatal Med 2020;33:3767-74. [Crossref] [PubMed]
- Avila-Alvarez A, Zozaya C, Pértega-Diaz S, et al. Temporal trends in respiratory care and bronchopulmonary dysplasia in very preterm infants over a 10-year period in Spain. Arch Dis Child Fetal Neonatal Ed 2022;107:143-9. [Crossref] [PubMed]
- García-Muñoz Rodrigo F, García Cruz L, Galán Henríquez G, et al. Variations in the number of births by day of the week, and morbidity and mortality in very-low-birth-weight infants. J Pediatr (Rio J) 2019;95:41-7. [Crossref] [PubMed]
- Solis-Garcia G, Avila-Alvarez A, García-Muñoz Rodrigo F, et al. Time at birth and short-term outcomes among extremely preterm infants in Spain: a multicenter cohort study. Eur J Pediatr 2022;181:2067-74. [Crossref] [PubMed]
- Valls-i-Soler A, Carnielli V, Claris O, et al. EuroNeoStat: a European information system on the outcomes of care for very-low-birth-weight infants. Neonatology 2008;93:7-9. [Crossref] [PubMed]
- Haumont D. NguyenBa C, Modi N. eNewborn: The Information Technology Revolution and Challenges for Neonatal Networks. Neonatology 2017;111:388-97. [Crossref] [PubMed]
- Available online: https://www.imperial.ac.uk/neonatal-data-analysis-unit/enewborn/enewborn-governanceadministration/
- Martin LJ, Sjörs G, Reichman B, et al. Country-Specific vs. Common Birthweight-for-Gestational Age to Identify Small for Gestational Age Infants Born at 24-28 weeks: An International Study. Paediatr Perinat Epidemiol 2016;30:450-61. [Crossref] [PubMed]
- Shah PS, Lui K, Sjörs G, et al. Neonatal Outcomes of Very Low Birth Weight and Very Preterm Neonates: An International Comparison. J Pediatr 2016;177:144-152.e6. [Crossref] [PubMed]
- Hines D, Modi N, Lee SK, et al. Scoping review shows wide variation in the definitions of bronchopulmonary dysplasia in preterm infants and calls for a consensus. Acta Paediatr 2017;106:366-74. [Crossref] [PubMed]
- Darlow BA, Lui K, Kusuda S, et al. International variations and trends in the treatment for retinopathy of prematurity. Br J Ophthalmol 2017;101:1399-404. [Crossref] [PubMed]
- Kelly LE, Shah PS, Håkansson S, et al. Perinatal health services organization for preterm births: a multinational comparison. J Perinatol 2017;37:762-8. [Crossref] [PubMed]
- Koller-Smith LI, Shah PS, Ye XY, et al. Comparing very low birth weight versus very low gestation cohort methods for outcome analysis of high risk preterm infants. BMC Pediatr 2017;17:166. [Crossref] [PubMed]
- Helenius K, Sjörs G, Shah PS, et al. Survival in Very Preterm Infants: An International Comparison of 10 National Neonatal Networks. Pediatrics 2017;140:e20171264. [Crossref] [PubMed]
- Beltempo M, Isayama T, Vento M, et al. Respiratory Management of Extremely Preterm Infants: An International Survey. Neonatology 2018;114:28-36. [Crossref] [PubMed]
- Darlow BA, Vento M, Beltempo M, et al. Variations in Oxygen Saturation Targeting, and Retinopathy of Prematurity Screening and Treatment Criteria in Neonatal Intensive Care Units: An International Survey. Neonatology 2018;114:323-31. [Crossref] [PubMed]
- Shah PS, Kusuda S, Håkansson S, et al. Neonatal Outcomes of Very Preterm or Very Low Birth Weight Triplets. Pediatrics 2018;142:e20181938. [Crossref] [PubMed]
- Shah PS, Lui K, Reichman B, et al. The International Network for Evaluating Outcomes (iNeo) of neonates: evolution, progress and opportunities. Transl Pediatr 2019;8:170-81. [Crossref] [PubMed]
- Shahroor M, Lehtonen L, Lee SK, et al. Unit-Level Variations in Healthcare Professionals' Availability for Preterm Neonates <29 Weeks' Gestation: An International Survey. Neonatology 2019;116:347-55. [Crossref] [PubMed]
- Lui K, Lee SK, Kusuda S, et al. Trends in Outcomes for Neonates Born Very Preterm and Very Low Birth Weight in 11 High-Income Countries. J Pediatr 2019;215:32-40.e14. [Crossref] [PubMed]
- Adams M, Bassler D, Darlow BA, et al. Preventive strategies and factors associated with surgically treated necrotising enterocolitis in extremely preterm infants: an international unit survey linked with retrospective cohort data analysis. BMJ Open 2019;9:e031086. [Crossref] [PubMed]
- Helenius K, Morisaki N, Kusuda S, et al. Survey shows marked variations in approaches to redirection of care for critically ill very preterm infants in 11 countries. Acta Paediatr 2020;109:1338-45. [Crossref] [PubMed]
- Norman M, Håkansson S, Kusuda S, et al. Neonatal Outcomes in Very Preterm Infants With Severe Congenital Heart Defects: An International Cohort Study. J Am Heart Assoc 2020;9:e015369. [Crossref] [PubMed]
- Gagliardi L, Rusconi F, Reichman B, et al. Neonatal outcomes of extremely preterm twins by sex pairing: an international cohort study. Arch Dis Child Fetal Neonatal Ed 2021;106:17-24. [Crossref] [PubMed]
- Lehtonen L, Lee SK, Kusuda S, et al. Family Rooms in Neonatal Intensive Care Units and Neonatal Outcomes: An International Survey and Linked Cohort Study. J Pediatr 2020;226:112-117.e4. [Crossref] [PubMed]
- Lui K, Vento M, Modi N, et al. Inter-center variability in neonatal outcomes of preterm infants: A longitudinal evaluation of 298 neonatal units in 11 countries. Semin Fetal Neonatal Med 2021;26:101196. [Crossref] [PubMed]
- Seaton SE, Draper ES, Adams M, et al. Variations in Neonatal Length of Stay of Babies Born Extremely Preterm: An International Comparison Between iNeo Networks. J Pediatr 2021;233:26-32.e6. [Crossref] [PubMed]
- García-Muñoz Rodrigo F, Fabres J, Tapia JL, et al. Factors Associated with Survival and Survival without Major Morbidity in Very Preterm Infants in Two Neonatal Networks: SEN1500 and NEOCOSUR. Neonatology 2021;118:289-96. [Crossref] [PubMed]
Cite this article as: San Feliciano L, Moro M, Figueras J, Sánchez Tamayo T, Zozaya C, García-Muñoz Rodrigo F, Vento M. The Spanish Neonatal Network SEN1500: updated information. Pediatr Med 2024;7:10.

