
The key social determinants of mental health: their effects among children globally and strategies to address them: a narrative review
Introduction
Recently, there has been an increase in mental health issues among children and adolescents around the world. Mental health is closely linked to what is termed physical health and is shaped by a child or teen’s social, economic, and local environment. Risk factors for many of the common mental disorders such as depression are heavily associated with social inequalities (1).
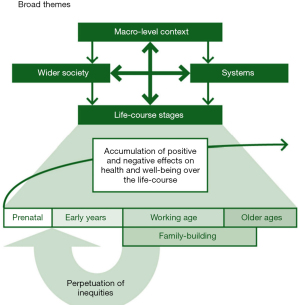
As seen in Figure 1, social inequalities that begin in childhood and adolescence can affect individuals over the life course. They can also be perpetuated from generation to generation. Addressing these inequalities early on is key. In this article, we review the associations between child and adolescent mental health and specific determinants of health including poverty, food security/nutrition, neighborhood/community, and trauma. We discuss racism as a more recently identified determinant of mental health. Finally, we review possible strategies to improving these important factors.
Methods
The authors conducted a literature review with a research database search using key words social determinants of health, child mental health adolescent mental health, social determinants of mental health, racism and child mental health. This search yielded a number of publications in the last 10 years and some foundational publications greater than 10 years in the past. These identified manuscripts were then evaluated to see if they referred to the social determinants of mental health for children and adolescents. The papers ultimately agreed upon by the authors to be used to complete the narrative review are referenced at the end of the manuscript.
Poverty and income inequality
Poverty is one of the social determinants of mental health that affects children and teens. Recent world events such as economic recessions, viral pandemics, political strife, refugee crisis, and natural disasters related to global warming have only increased the likelihood of children growing up in poverty or in communities with income inequality around the world.
Globally, almost 1.2 billion people live in extreme poverty and lack basic security in areas such as employment, housing, health care, and education. Globally, most people living below the poverty line are in Southern Asia or sub-Saharan Africa. In addition, high poverty rates are found in small, fragile, and conflict-affected countries (2). According to the American Psychological Academy, living in poverty can be associated with negative conditions such as food insecurity and substandard housing. Also, it is linked to problems such as inadequate nutrition, limited health care and unsafe neighborhoods (3). These factors in turn may affect physical and emotional wellbeing. More specifically, children and teens who are from lower socioeconomic backgrounds are at greater risk for poor academic achievement, behavioral issues, physical health problems, and developmental delays.
Poverty and academic attainment
Living in poverty has also been demonstrated to negatively affect children’s focus and memory. For example, in one study involving poverty and child health, researchers at Cornell University tracked 341 children for over 15 years. Short-term spatial memory was evaluated by having participants press colored pads in a specific order to repeat a sequence of sounds and lights. Researchers noted that study participants who grew up in poverty were more likely to have decreased short-term spatial memory and not able to perform this task at the same level as participants from middle-income backgrounds. Researchers also noted that children who live in poverty were at higher risk of experiencing chronic stress which could continue to affect them through adulthood (4).
Poverty and psychosocial outcomes
In a study conducted among underprivileged children in rural China, researchers reviewed school-based surveys of nearly 1,300 children in grades 4–9. They concluded that poverty had a significant correlation with subject’s mental health. Also, that family and peers had a mediating effect on poverty and children’s mental health (5).
Research shows that children and teens in low-income families are at higher risk of behavioral and psychological issues. Examples include impulsiveness, attention deficit hyperactivity disorder (ADHD), anxiety, depression, and poor self-esteem. Children living in poverty also had a greater likelihood of antisocial conduct such as bullying as well as helplessness behavior, than kids from more affluent backgrounds (3).
Of note, while these are behavioral risks that have been associated with being poor and emerge while being studied, the data do not support that these findings will always lead to behavioral problems. Context and environmental influences must be taken into consideration as well.
Poverty and physical health
Being poor can also influence the developing brain. For example, growing up in poverty is associated with smaller white matter and cortical grey matter as well as hippocampal and amygdala volumes in children (6). Children and teens living in low-income situations are also at increased risk for number of physical health problems such as asthma, and anemia (7).
As will be discussed later, lack of access to healthy foods can lead to children being overweight or obese. In addition, exposure to environmental contaminants in the neighborhood and community such as lead in the water supply or in paint and toxic waste dumps can affect health. These effects are often worsened by the difficulties that less affluent children and their families face when trying to obtain regular health care.
Income inequality and wellbeing
Globally, children and teens in lower socioeconomic groups are less likely to experience conditions that allow for optimal health and development. For example, at the macrolevel, having income inequality can be associated with higher BMI’s, more psychological symptoms, and decreased life satisfaction (7,8). Analysis from the United Kingdom also shows that there is an inverse relationship between family income and socioemotional difficulties among young children. However, this negative impact can be mitigated by positive parenting activities and healthy social and emotional bonds (9).
Food insecurity and malnutrition
Food insecurity is defined as inadequate access to safe, sufficient and nutritious food that meets one’s dietary needs (10). Malnutrition refers to deficiencies or imbalances in intake of energy or nutrients. The term malnutrition covers both ‘undernutrition’—which includes stunting (low height for age), wasting (low weight for height), underweight (low weight for age) and micronutrient deficiencies (a lack of important vitamins and minerals), as well as, ‘overnutrition’ which includes being overweight or obese.
Food insecurity and malnutrition affect millions of infants, children, and teens around the world. The COVID-19 pandemic has unfortunately been linked to an increase in the number of children and youth who suffer from hunger. Food insecurity and malnutrition are associated with poorer mental health outcomes among children and teens.
Food insecurity and mental health
Food insecurity is associated with increased mental health concerns and exists in both high and low income countries. In a UNICEF study conducted between 2014–2015, 41% of children under age 15 lived with an adult who faced moderate or severe food insecurity and 19% lived with an adult who faced severe food insecurity. Overall, one in 10 children in the countries surveyed lacked access to safe, sufficient and nutritious foods (11).
In another UNICEF study involving 147 countries, food insecurity was assessed using the Food Insecurity Experience Scale Survey Module for Individuals. In this study, indices of mental health were also calculated based participants’ recent experiences with depression and mental distress. Of note, the prevalence of food insecurity ranged from almost 20% in East Asia to nearly 76% in Sub-Saharan Africa. Importantly, food insecurity was associated with lower mental health among all respondents (12).
Food insecurity and access to health care
In addition to poorer mental health, household food insecurity is also associated with poorer healthcare access along with more acute and chronic health problems. A US based study conducted by Thomas et al, using nationally representative data from waves of the National Health Interview Study (n=29,341) examined a broad range of child health outcomes among children 2 to 17 years old. Children in food-insecure households as compared to those who were not food insecure had lifetime depressive symptoms that were 19.1% and 27.9% higher, and rates of emergency department use that were 25.9% higher. The study authors suggest that policies used to reduce household food insecurity among children may also reduce children’s chronic and acute health problems and health care needs (13).
Maternal over and under nutrition and child health
Maternal undernutrition and a low pregnancy BMI can be a risk factor for poor birth outcomes. Maternal overnutrition, on the other hand, with high intake of processed foods during pregnancy can also predict poor mental health outcomes in children and teens.
Research shows that having an adequate nutritional intake during pregnancy is key for neurodevelopment and a normal birth weight. For example, Vitamin A deficiency can cause severe preventable blindness in children (14). Thus, it is important to ensure sufficient intake of Vitamin A along with Iron, Choline, B12, Zinc, Tryptophan, Omega-3s, Iodine and Iron during pregnancy. In fact, increasing intake of some nutrients such as choline consumption during pregnancy has been shown to alleviate poor social interactions and improve anxiety such as behavior in animal models (15).
Malnutrition and cognitive development
In low-income countries, approximately 30 million infants are born every year with impaired growth due to poor nutrition during pregnancy. Malnutrition in infants and children affects cognitive development during the early years. Poor fetal nutrition has also been strongly associated with chronic disease in adulthood (16). What is concerning is that the effects of malnutrition during the first two years of life is mostly irreversible. Research shows that children with poor nutrition tend to enter primary school later, drop out earlier and are overall less able to learn than peers who have received better nourishment (14). Therefore, addressing infant and child malnutrition may have a long-term benefit on development and health.
Neighborhood or community
In addition to factors such as poverty and food insecurity, a child or adolescent’s neighborhood or community can significantly affect their mental and behavioral health. This includes environmental factors, such as exposure to violence or physical surroundings, from broken windows to air pollutants. Also, geographical factors such as the distance of the neighborhood to good jobs or the availability to resources such as schools and medical clinics in the neighborhoods can have a connection to individual outcomes and child mental health (17).
Pollution and mental health
Pollution can affect physical and mental health. For example, prenatal exposure to air pollutants has been associated with reduced left hemisphere white matter volume in school aged children (18). It has also been linked with slower processing speeds, ADHD, and other externalizing symptoms.
In many parts of the world, children and adolescents are exposed to regular noise, dust, and pollutants secondary to roadside traffic. According to a UK study, exposure to air pollution caused by construction and traffic among children can increase the likelihood of major depression later. Researchers in this study found that children and adolescents growing up in areas of London with high air pollution were more likely by age 18 to have depression and other mental health disorders than their peers raised in areas with cleaner air. When subjects were divided into groups, based on the quality of air they were exposed to until 10 years of age, researchers found the bottom seventh—who experienced the worst air—had 29 percent, 148 percent, 51 percent and 162 percent higher rates for bipolar, schizophrenia, depression and personality disorder, respectively, than the top seventh who had experienced the cleanest air.
There are several explanations for how mental health is affected by air pollution. In one theory based on animal studies, inflammation in the respiratory tract leads to inflammation across the body extending into the brain. In another, air pollutants travel from the nose to the brain where they accumulate and cause damage (19).
There are many places around the world, such as in New Delhi and Beijing where children and teens are exposed to high levels of air pollution on a regular basis. According to WHO, if a child is exposed to significant air pollution they are at higher risk for delayed brain development and chronic respiratory diseases, as well as, having cancers or stroke in adulthood.
Access to green space and ADHD
In urban locations such as Hong Kong and New York City, children and teens have reduced access to green space and nature. However, research shows that access to green spaces may have a beneficial effect on mood and behavioral issues. For example, studies show that childhood ADHD symptoms can be decreased by spending time in nature. Also, that “green time” may be an integral addition to established pharmacological and psychological treatments.
Researchers have shown that kids who played in indoor settings without windows had a higher level of symptoms than those who played in green outdoor spaces (20). Also that teens and children with ADHD had better scores on concentration tests after exposure to urban settings with some nature as compared to city settings without nature (21).
Unsafe neighborhoods and mental health
Unsafe neighborhoods may expose children to violence such as bullying, interpersonal, community and law enforcement violence, which can cause other psychosocial issues. Low-income neighborhoods that experience violence in comparison to middle class or higher neighborhoods who experience violence, may have less community resources to respond and address the underlying causes leading to longer-term effects from repeated unaddressed violent actions. Exposure to violence in a child’s community can lead to complex post-traumatic stress disorder, trauma, injury, disability, and death. Violence exposure among children and teens may be associated with subsequent violent behavior. This in turn puts young people at risk for injury and placement in the juvenile justice system (22).
The effects of peer groups among disadvantaged teens is significant. Studies have shown a strong correlation between teens having peers that are a negative influence and teens having lower grades plus increased antisocial behavior (17). However, positive relationships (whether by peer, parent, or teacher) along with spirituality can be protective. In a study of children in an African American community with high rates of community violence, complex PTSD caused by exposure to violence was buffered and moderated by formal kinship relationships and spirituality as well as other combined supports (23).
Trauma
Adverse childhood events (ACEs) are early traumatic events that can lead to toxic stress and impact adult health. Toxic stress is related to threats that are severe or ongoing—such as abuse, neglect or having a parent who has an untreated mental disorder (24).
Toxic stress, brain development and the immune system
When the stress response is overstimulated it can affect brain development, the immune system and how DNA is transcribed. More specifically, high doses of stress hormones can affect the brain’s executive functioning. This can be seen on imaging studies as a shrinking of the hippocampus which is the brain area that controls memory and emotional regulation, along with an increase in the size of the amygdala also know as the brain’s fear center (24).
The pleasure and reward region of the brain can be significantly affected among children who are exposed to high number of adverse events in childhood. As a result, these individuals may feel less pleasure and need higher and higher doses to feel pleasure, which may in turn lead to risky behaviors and substance dependence. In addition to affecting brain development, ACEs can impact the immune system and put teens at risk for chronic inflammation and autoimmune diseases such as asthma. According to one article, a child or teen with four or more ACEs has twice the risk for asthma as a person with no ACEs (25).
ACEs and premature cellular aging
ACEs can affect the way DNA is read and created. More specifically, exposure to ACEs can cause telomeres, which protect DNA from wear and tear, to shorten and cause premature cellular aging. Risk is related to the total exposure to adversity and whether there was a caregiver who could decrease the effect of that chronic stress (25).
Trauma and medical conditions
Traumatic experiences in childhood have been associated with having more medical conditions throughout the one’s life. The ACE study is a longitudinal study that examines the effect of childhood trauma into adulthood. The study involved nearly 17,000 participants ranging from ages 19 to 90. Researchers in this study collected subjects’ medical histories over time along with their childhood exposure to abuse, violence, and impaired caregivers. Of note, nearly 2/3rds of participants experienced at least one exposure, and of those, nearly 70% reported two or more incidents of childhood trauma. Results of the study clearly showed the association between childhood trauma exposure with high-risk behaviors (e.g., smoking), chronic illness, and early death (26).
Racism
Racism is defined as a belief that race (that is, how one looks) is the primary determinant of human traits, abilities and rights and that racial differences (such as skin color) produce an inherent superiority of a particular group. Although racism as a term is relatively new, the concept has existed in many communities globally. Racism has increasingly been viewed as a social determinant affecting child mental health. In the past, the idea that racism impacted the health and wellbeing of children and adults was viewed as debatable. A common theme was that if poverty were eliminated, racial differences in wellbeing would also dissolve and that racism was not by itself causing issues outside of poverty. More recently racism has been highlighted as a factor that independently has profound effect on the lives of children and teens in many countries. In fact, pervasive racism is currently being called a public health emergency in the US (27).
Racism, education, and wages
Redlining refers to concept of where a person of a specific race is prevented from living or purchasing a home outside of a designated area. Racism and redlining continue to be significant determinants of where black and brown people can live. These factors can impact the educational system and affect employment and wages. Of note, intentional, institutional barriers limit the potential of black and brown families from getting certain jobs and higher salaries (28).
In the US, it has been shown that differences in jobs and salaries persist regardless of education, with female African American women receiving the most discrepancy in pay compared to their counterparts in employment. Lower wages paired with insufficient resources lead to lower education potential, food insecurity, unsafe neighborhoods, increased family instability, higher maternal death, and poorer financial status regardless of education.
Racism and mental health
Racism has been shown to correlate with poorer mental health including depression, anxiety, and psychological stress, as well as decreased physical health (29). A review of multiple studies found that adolescents who reported experiencing discrimination had a higher likelihood of developing mental health problems such as depression compared to teens who did not (30). A recent study among Asian-American college students who completed daily surveys of race-related stressors and physical health showed that when subjects experienced “racial microaggressions” or mistreatment they reported lower sleep quality and duration the following day (31).
Social determinants of health are amplified by structural racism in the US. While there have been many theoretical assertions of moderators, the relationship among racial group socioeconomic status, age, and gender still need to be examined further. In 2019, the American Academy of Pediatrics in the United States published a policy statement formally acknowledging the impact of racism on the wellbeing of children and adolescents (32). Of course, racism and its negative effects is not limited to the US. Around the world, researchers are looking at the impact of phenotype (how one looks) and other race-based factors on child health in their countries and finding similar results (33).
Key strategies for addressing social determinants of mental health
General concepts
According to a 2014 World Health Organization (WHO) review (9), the following concepts need to be taken into consideration when addressing social determinants and mental health:
(I) Use a life course approach
A life-course perspective indicates that health at each stage of life is affected by both unique and common factors.
(II) Focus on early intervention to improve health
Programs, particularly in low- and middle-income countries, that intervene early in a child’s life can prevent both acute and long term mental health issues. This approach also helps children and adolescents maximize their potential and to thrive.
(III) Address physical health to optimize mental health
More specifically, decreasing inequalities in mental health attainment cannot occur without addressing barriers related to addressing the health of the whole child. Providing comprehensive care for acute and chronic physical illness can help prevent mental health issues.
(IV) Prioritize mental health and ensure mental health equity in all policies
There is a clear need globally for mental health to have greater focus and recognition. This is true in low- and middle-income countries, where lack of resources are notable, but of note, there are also challenges in high income countries related to access to mental health services, payment structures and stigma.
(V) Implement action at both the local and country wide level
Finally, reducing inequalities in mental health is a task that must be addressed on a local level, as well as, nationally. Country-level strategies are most likely to have a significant impact on decreasing inequalities. A wide range of actions at the national level, including alleviating poverty, implementing effective social protection across the life-course, reducing discrimination, preventing violent conflict, and promoting access to health care, housing, and education, can lead to significant benefits in mental health across a population.
Specific strategies for addressing social determinants
The following are some more specific strategies to consider for addressing poverty, food insecurity, family/neighborhood and community related issues, trauma, and racism.
Poverty
Poverty may affect a family’s ability to provide a safe and healthy environment for their child. Parental employment and access to quality education can play significant roles in support of families and their children (9).
Families, neighborhoods, and communities
Schools play a significant role in the development of social, emotional, academic, and cognitive ability. Actions to address children and teen mental health disorders within school settings have been implemented successfully in countries across the world (9). Notable are school-based interventions in communities affected by violence where the chances of acquiring mental health problems are especially high.
Regarding community space, a recent study reviewing the evidence on the effects of green space in urban areas shows that these spaces offer benefits such as psychological relaxation and stress reduction, in addition to decreasing air pollution. Therefore there is a need for small green spaces close to where people live and larger spaces such as parks, that provide formal recreational facilities (34).
It is also crucial to ensure safe and healthy surroundings, as the environment has a profound influence on children’s growth and development. To provide a healthy environment for children, the WHO recommends improving sanitation, reducing air pollution, and building safer environments (11).
Malnutrition and food insecurity
Eliminating food “deserts” and increasing access to low-cost, healthy foods early on and throughout childhood and adolescence is essential. Promoting breastfeeding is one of the best ways to protect babies. Maternal nutrition is critical and elimination of diets deficient in essential nutrients can support a healthy pregnancy and an infant’s physical and mental health. In a recent trial in Nepal, the use of low-dose vitamin A supplements reduced maternal mortality by 44% and was a low-cost strategy to improving pediatric outcomes (35).
Studies also show that community-based approaches are needed to strengthen household food security. Community wide awareness programs are needed to raise the alert on the importance of health and nutrition. For example, there is a need to ensure a sustainable, adequate intake of iodine by all adolescent girls and women of childbearing age prior to conception to prevent mental retardation and iodine deficiency. This can be accomplished in the long run by using iodized salt and fortified foods such as bread (9).
Trauma
It is common for children and teens to be exposed to more than a single traumatic event and children exposed to chronic trauma are especially vulnerable to the impact of additional trauma. When families come to the attention of professionals, the specific trauma needs to be attended to but also essential is gathering a thorough, detailed history of all trauma exposure throughout the life course and the provision of comprehensive psychological support (24).
Racism
Finally, reviewing and revising policies that perpetuate institutionalized racism in the systems of healthcare, housing, education, and the economy in particular will begin to address the pervasive impact of differential and unequal treatment on the mental health and wellbeing of children and adolescents worldwide (36).
Conclusions
From this review, we conclude that there is considerable evidence that addressing mental health and reducing the risk of conditions associated with poverty, food insecurity, unsafe neighborhoods, trauma, and racism has significant benefits for children and teens. Therefore, it is essential that researchers, health professionals, policy makers and other stakeholders ensure comprehensive steps are taken globally by: considering a life course approach, focusing on early intervention, addressing the health of the whole child, ensuring mental health equity in all policies, and implementing actions to address social determinants at both the local and country wide level.
Acknowledgments
We would like to thank McKenna Pho for her assistance with editing this manuscript.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Danielle Laraque-Arena and Ruth E. K. Stein) for the series “Integrating Mental Health in the Comprehensive Care of Children and Adolescents: Prevention, Screening, Diagnosis and Treatment” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://pm.amegroups.com/article/view/10.21037/pm-20-78/coif). The series “Integrating Mental Health in the Comprehensive Care of Children and Adolescents: Prevention, Screening, Diagnosis and Treatment” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Berry OO, Londoño Tobón A, Njoroge WFM. Social Determinants of Health: the Impact of Racism on Early Childhood Mental Health. Curr Psychiatry Rep 2021;23:23. [Crossref] [PubMed]
- Maxwell S. The meaning and measurement of poverty. London: Overseas Development Institute, 1999.
- American Psychological Association. Effects of poverty, hunger and homelessness on children and youth. American Psychological Association, 2009. Available online: https://www.apa.org/pi/families/poverty
- Kelley, S. For kids, poverty means psychological deficits as adults. Cornell Chronicle. 2016 Dec. Available online: https://news.cornell.edu/stories/2016/12/kids-poverty-means-psychological-deficits-adults
- Li C, Wu Q, Liang Z. Effect of poverty on mental health of children in rural China: the mediating role of social capital. Applied Research in Quality of Life 2019;14:131-53. [Crossref]
- Luby J, Belden A, Botteron K, et al. The effects of poverty on childhood brain development: the mediating effect of caregiving and stressful life events. JAMA Pediatr 2013;167:1135-42. [Crossref] [PubMed]
- Effects of poverty, hunger and homelessness on children and youth. Available online: https://www.apa.org/pi/families/poverty
- Elgar FJ, Pförtner TK, Moor I, et al. Socioeconomic inequalities in adolescent health 2002-2010: A time-series analysis of 34 countries participating in the Health Behaviour in School-aged Children study. Lancet 2015;385:2088-95. [Crossref] [PubMed]
- World Health Organization & the Calouste Gulbenkian Foundation. Social determinants of mental health. World Health Organization, 2014. Available online: https://www.who.int/mental_health/publications/gulbenkian_paper_social_determinants_of_mental_health/en/
- Melchior M, Chastang JF, Falissard B, et al. Food insecurity and children's mental health: a prospective birth cohort study. PLoS One 2012;7:e52615. [Crossref] [PubMed]
- Pereira A, Diego-Rosell. Hunger knows no boundaries. 2017 Sept 28. In: Gallup Blog. Gallup. 2017. Available online: https://news.gallup.com/opinion/gallup/219965/hunger-knows-no-boundaries.aspx
- Jones AD. Food insecurity and mental health status: A global analysis of 149 countries. Am J Prev Med 2017;53:264-73. [Crossref] [PubMed]
- Thomas MMC, Miller DP, Morrissey TW. Food Insecurity and Child Health. Pediatrics 2019;144:e20190397. [Crossref] [PubMed]
- United Nations Population Fund. Health and the links to nutrition: Maternal health is key. 2004 Mar 22. Available online: https://www.unfpa.org/press/health-and-links-nutrition-maternal-health-key
- Blusztajn JK, Mellott TJ. Neuroprotective actions of perinatal choline nutrition. Clin Chem Lab Med 2013;51:591-9. [Crossref] [PubMed]
- Sawaya AL, Martins P, Hoffman D, et al. The link between childhood undernutrition and risk of chronic diseases in adulthood: a case study of Brazil. Nutr Rev 2003;61:168-75. [Crossref] [PubMed]
- Galster GC. How neighborhoods affect health, well-being, and young people’s futures. Macfound.org: MacArthur Foundation. 2014 Mar. Available online: https://www.macfound.org/media/files/HHM_-_Neighborhoods_Affect_Health_Well-being_Young_Peoples_Futures.pdf
- Peterson BS, Rauh VA, Bansal R, et al. Effects of prenatal exposure to air pollutants (polycyclic aromatic hydrocarbons) on the development of brain white matter, cognition, and behavior in later childhood. JAMA Psychiatry 2015;72:531-40. Erratum in: JAMA Psychiatry 2015;72:625. [Crossref] [PubMed]
- South China Morning Post. Air pollution linked to mental health problems in children, new study finds. 2019. Available online: https://www.scmp.com/news/world/europe/article/3023665/air-pollution-linked-mental-health-problems-children-new-study
- Taylor AF, Kuo FE, Sullivan WC. Coping with ADD - The surprising connection to green play settings. Environ Behav 2001;33:54-77. [Crossref]
- Kuo FE, Taylor AF. A potential natural treatment for attention-deficit/hyperactivity disorder: evidence from a national study. Am J Public Health 2004;94:1580-6. [Crossref] [PubMed]
- Children Exposed to Violence | National Institute of Justice. Available online: www.ojp.gov
- Sanders-Phillips K. Racial discrimination: a continuum of violence exposure for children of color. Clin Child Fam Psychol Rev 2009;12:174-95. [Crossref] [PubMed]
- Abraham A. Raising Global Teens. Summertime Publishing, 2020.
- Bornstein D. Treating the lifelong harm of childhood trauma. The New York Times. 2018 Jan 30. Available online: https://www.nytimes.com/2018/01/30/opinion/treating-the-lifelong-harm-of-childhood-trauma.html
- NCRSN. The National Child Traumatic Stress Network. Effects. Available online: https://www.nctsn.org/what-is-child-trauma/trauma-types/complex-trauma/effects
- Jones CP. Addressing Violence Against Children Through Anti-racism Action. Pediatr Clin North Am 2021;68:449-53. [Crossref] [PubMed]
- Dreyer BP, Trent M, Anderson AT, et al. The Death of George Floyd: Bending the Arc of History Toward Justice for Generations of Children. Pediatrics 2020;146:e2020009639. [Crossref] [PubMed]
- Paradies Y, Ben J, Denson N, et al. Racism as a Determinant of Health: A Systematic Review and Meta-Analysis. PLoS One 2015;10:e0138511. [Crossref] [PubMed]
- Priest N, Paradies Y, Trenerry B, et al. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med 2013;95:115-27. [Crossref] [PubMed]
- Psychology Today. How does racism affect health? Psychology Today; 2020 Jun 4. Available online: https://www.psychologytoday.com/us/blog/evidence-based-living/202006/how-does-racism-affect-health
- Trent M, Dooley DG, Dougé J, et al. The Impact of Racism on Child and Adolescent Health. Pediatrics 2019;144:e20191765. [Crossref] [PubMed]
- Boyer Y. Healing racism in Canadian health care. CMAJ 2017;189:E1408-9. [Crossref] [PubMed]
- Hedblom M, Gunnarsson B, Iravani B, et al. Reduction of physiological stress by urban green space in a multisensory virtual experiment. Sci Rep 2019;9:10113. [Crossref] [PubMed]
- Center for Global Development. Gottlieb J. Case 4: Reducing child mortality with vitamin A in Nepal. 2001. Available online: https://www.cgdev.org/page/case-4-reducing-child-mortality-through-vitamin-nepal
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US), 2003.
Cite this article as: Abraham A, Walker-Harding L. The key social determinants of mental health: their effects among children globally and strategies to address them: a narrative review. Pediatr Med 2022;5:7.

